A 63-year-old man presented with decreased vision, which he attributed to a cataract “growing” over his eye during the past year. His medical history contained nothing significant.
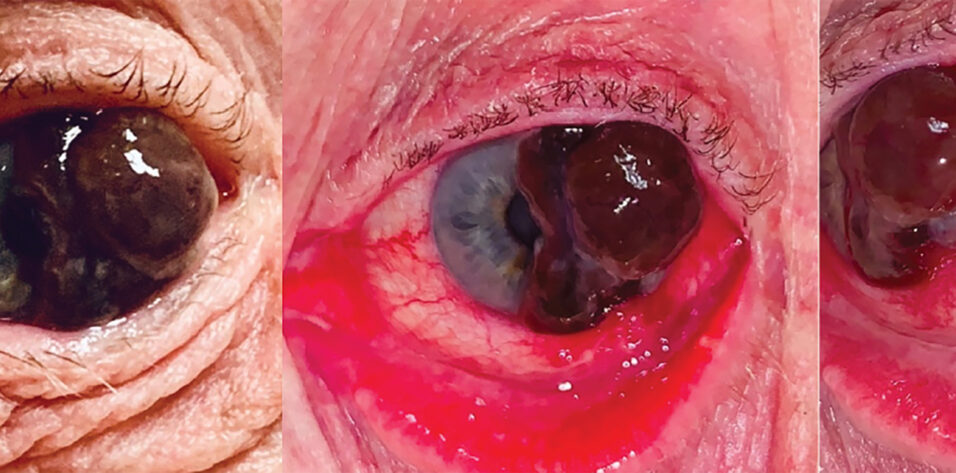
Upon examination, a large pigmented conjunctival lesion extending from the temporal perilimbal conjunctiva over the cornea was observed (Figure). The lesion partially obscured the visual axis and disrupted normal eyelid function. Marked inflammation of the surrounding conjunctiva and prominent feeder vessels were noted. The lesion’s nodular appearance and size, corneal involvement, and associated vessels were highly suggestive of conjunctival melanoma.
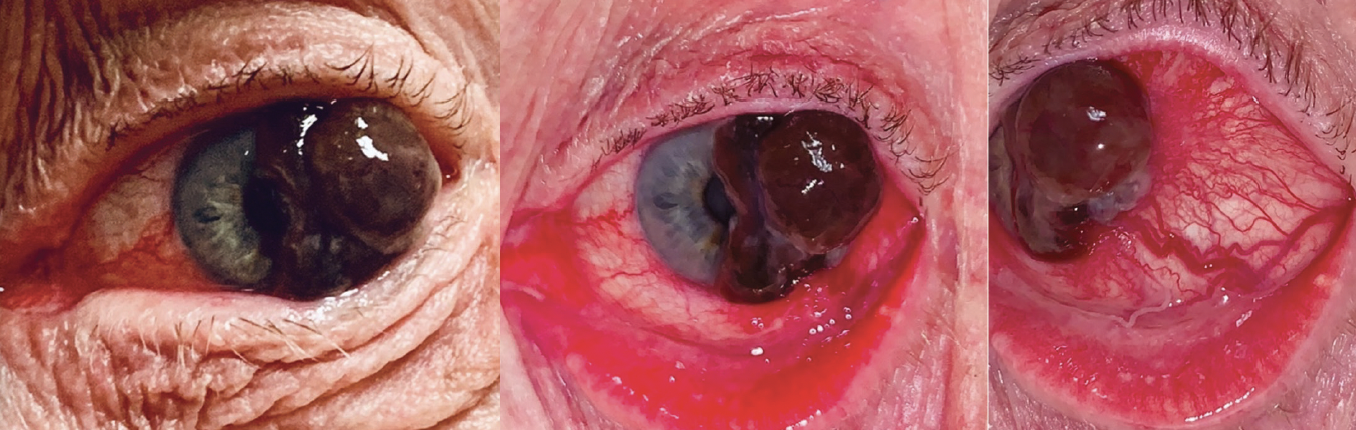
Figure. A large, pigmented, conjunctival lesion with prominent feeder vessels extends from the temporal perilimbal conjunctiva over the cornea.
EPIDEMIOLOGY AND RISK FACTORS
At 0.39 per million individuals, the incidence rate of conjunctival melanomas in the United States is relatively low.1 These tumors most frequently occur in White patients (91% of cases). The incidence increases with age. A large retrospective study found that 76% of conjunctival melanomas arose from primary acquired melanosis (PAM), 15% developed de novo, and 9% originated from conjunctival nevi.2
The etiology of the patient’s lesion remains uncertain based on his medical history.
STANDARD TREATMENT PROTOCOLS
The standard treatment for suspected conjunctival melanoma includes excisional biopsy with 3- to 5-mm margins and an amniotic membrane graft. A dry, no-touch technique is essential during excision; balanced salt solution should not be used, and direct contact with the lesion should be avoided to minimize the spread of melanoma cells.3 An alcohol epitheliectomy is also performed for corneal involvement. Care is taken to ensure Bowman membrane remains intact because it acts as a natural barrier against deeper tumor invasion. After excision, cryotherapy using a double-freeze-thaw cycle is performed at the lesion’s edges, and alcohol is applied to the scleral base. Any additional areas of PAM showing atypia beyond the primary lesion’s margins are also excised to prevent recurrence. If the PAM is diffuse or the surgical margins are positive, topical mitomycin C may be administered postoperatively, but the antifibrotic agent should not be used as primary therapy because of its inability to penetrate the basement membrane.4
Systemic evaluation by a medical oncologist is necessary. Although the utility of lymphoscintigraphy and sentinel lymph node biopsy remains controversial, these procedures may be considered in high-risk cases.4,5
PROGNOSTIC FACTORS AND FUTURE DIRECTIONS
The prognosis for conjunctival melanoma is generally unfavorable. Multiple studies have found an average local recurrence rate of 40% within an average follow-up period of 2.4 years. The rates of lymph node and systemic metastases were 19% over an average of 3.4 years. Likewise, melanoma-related mortality averaged 18% over a 4.9-year follow-up period.4
The preauricular nodes are often the first site of metastatic spread. In one study, however, 26% of patients with distant metastases showed no evidence of prior or concurrent regional lymph node involvement.5 Several factors are associated with a poor prognosis; these include involvement of nonbulbar conjunctiva, tumor thickness exceeding 2 mm, a de novo origin, nodular growth pattern, incomplete surgical excision, and histologic evidence of ulceration.4
At present, there is no standardized chemotherapy regimen for advanced conjunctival melanoma. It is important to note that this form of melanoma is genetically distinct from uveal melanoma. The former exhibits clinical behaviors and mutation patterns—specifically in the BRAF, NRAS, and KIT genes—similar to cutaneous melanoma.6,7 Several small case studies have evaluated the application of targeted molecular therapies such as BRAF and MEK inhibitors as well as immune checkpoint inhibitors such as anti-PD1 and anti–CTLA-4 agents, which are used in the treatment of cutaneous melanoma.8,9 The results were encouraging. The rarity of this tumor type, however, means that less is known about its behavior compared to cutaneous melanomas. Further research is needed.
CONCLUSION
Conjunctival melanoma is a relatively uncommon malignancy that carries a generally poor prognosis. Early recognition of and intervention for PAM lesions are crucial to prevent progression to conjunctival melanoma. The primary treatment modality is surgical excision, complemented by cryotherapy and alcohol application. Given the high rates of lymph node and systemic metastases, all patients should be referred to a medical oncologist for further evaluation and treatment. Because of the genetic and behavioral similarities between conjunctival and cutaneous melanomas, there is an emerging role for targeted therapies and immune checkpoint inhibitors, but additional research is required to ascertain the most effective treatment options.
1. Weppelmann TA, Zimmerman KT, Rashidi V. Trends in incidence of conjunctival melanoma in the US. JAMA Netw Open. 2022;5(10):e2237229.
2. Pacheco RR, Yaghy A, Dalvin LA, et al. Conjunctival melanoma: outcomes based on tumour origin in 629 patients at a single ocular oncology centre. Eye (Lond). 2022;36(3):603-611.
3. Shields JA, Shields CL, Mashayekhi A, et al. Primary acquired melanosis of the conjunctiva: experience with 311 eyes. Trans Am Ophthalmol Soc. 2007;105:61-71; discussion 71-72.
4. Wong JR, Nanji AA, Galor A, Karp CL. Management of conjunctival malignant melanoma: a review and update. Expert Rev Ophthalmol. 2014;9(3):185-204.
5. Esmaeli B, Wang X, Youssef A, Gershenwald JE. Patterns of regional and distant metastasis in patients with conjunctival melanoma: experience at a cancer center over four decades. Ophthalmology. 2001;108(11):2101-2105.
6. Griewank KG, Westekemper H, Murali R, et al. Conjunctival melanomas harbor BRAF and NRAS mutations and copy number changes similar to cutaneous and mucosal melanomas. Clin Cancer Res. 2013;19(12):3143-3152.
7. Beadling C, Jacobson-Dunlop E, Hodi FS, et al. KIT gene mutations and copy number in melanoma subtypes. Clin Cancer Res. 2008;14(21):6821-6828.
8. Sagiv O, Thakar SD, Kandl TJ, Ford J, Sniegowski MC, Hwu WJ, Esmaeli B. Immunotherapy with programmed cell death 1 inhibitors for 5 patients with conjunctival melanoma. JAMA Ophthalmol. 2018;136(11):1236-1241.
9. Peil J, Bock F, Kiefer F, et al. New therapeutic approaches for conjunctival melanoma-what we know so far and where therapy is potentially heading: focus on lymphatic vessels and dendritic cells. Int J Mol Sci. 2022;23(3):1478.