Abstract
Periorbital infections lead to severe condition of the orbital abscess, and eventually to sight loss, and even death. Current study aims in reviewing the literature regarding orbital abscess in adult patients and presenting 2 original cases. A surgical intervention to drain the abscess and a revision of the orbital was required. A review of literature is also reported focusing on aetiology and treatment options dealing with an orbital abscess.
Similar content being viewed by others
Introduction
Periorbital infections lead to severe condition of orbital abscess, and eventually to sight loss, and even death [1, 2]. They carry the risk of rapid deterioration, hence require immediate management [3].
In 1970, Chandler et al. proposed the classification of orbital complications depending on its extention: I—preseptal cellulitis; II—orbital cellulitis; III—subperiosteal abscess; IV—orbital abscess; V—cavernous sinus thrombosis [4]. Current study aims in reviewing literature regarding orbital abscess in adult patients and presenting 2 original cases.
Case Report 1
A 35-year-old woman presented to the maxillofacial surgery department in Poznań due to massive eyelid swelling and severe pain in the left eye. Three days before the patient was admitted to the department, she was injured with a blunt instrument. The physical examination shows massive swelling of the eyelids of the left eye—closing the eyelid gap, exophthalmos of the left eyeball, severe pain on palpation, redness and warming of the surrounding soft tissues, eruptions on the skin of the upper and lower eyelids, body temperature 37.9 °C (Fig. 1). No other irregularities were found. Computed tomography of the orbital without contrast and an X-ray of the lungs, laboratory tests, electrocardiogram were ordered. Additional a smear was taken for bacteriological examination. The computed tomography image shows phlegmon of the left cheek and orbital (Fig. 2). In the ophthalmological examination, the right eye remained unchanged. In the left eye, there was an abscess of the eyelids and orbit, swelling of the eyeball and eyelid conjunctiva; transparent cornea; iris unchanged; the pupil is even, round and reacts correctly to light. The image of the fundus of the right eye was normal, the left eye was not available for examination. The patient was administered amoxicillin and clavulanic acid 1.2 g intravenous (IV) three times a day, Metronidazole 500 mg three times daily IV, ketoprofen 0.1 g twice daily, enoxaparin 0.4 ml once daily subcutaneous. Additionally, drops containing dexamethasone and tobramycin every two hours were used for the left eye. Under general endotracheal anaesthesia, an incision and drainage of the left orbital phlegmon were performed from the supraorbital and suborbital incisions, resulting in abundant purulent exudate (Fig. 3). The abscess cavity was rinsed with saline. A flow drain was introduced. In the postoperative period, the level of CRP and WBC was monitored—a decrease in CRP and WBC was observed. On the third day after surgery, a control ophthalmological examination confirmed correct vision in the left eye (Fig. 4). The microbiological examination revealed the alarm pathogen Streptococcus pyogenes susceptible to empirical therapy, Staphylococcus aureus, Staphylococcus epidermidis. The patient was discharged from the clinic on day 9 in good general condition. There were no visual disturbances in the left eye. The only permanent consequence was scarring of the facial skin after surgical access (Fig. 5).
Case Report 2
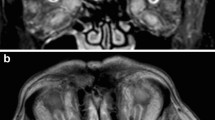
A 63-year-old man was transferred from the department of ophthalmology to the department of maxillofacial surgery due to blindness in the left eye due to orbital phlegmon in order to decompress the abscess. 8 days before hospitalization, the patient suffered a facial injury as a result of hitting a metal gate. Immediately after the injury, the skin wound was treated at the ophthalmology department. Symptoms of acute inflammation appeared on the 5th day after the injury. Physical examination shows a contaminated, extensive wound to the skin of the upper eyelid and the left supraorbital area, penetrating the orbital along the roof and the sidewall, from which the exudate of the purulent content emerges. Left eye exophthalmos, the blindness of the left eye, significantly limited mobility of the left eyeball. Due to the swelling, the palpebral fissure was narrowed. Disturbed sensation in the area of the left orbital. Fracture in the craniofacial skeleton was not detected (Fig. 6). Body temperature was normal. The patient does not report comorbidities and allergies. The patient does not take medications and does not mention any social problems. Magnetic resonance imaging orbitals was performed, which showed an image of an abscess of the left orbit, exophthalmos and a forced course of the optic nerve (Fig. 7). Additionally, a craniofacial CT scan, lung X-ray, ECG were performed, a smear was taken for bacteriological examination and blood was taken for laboratory tests. The patient was administered ceftriaxone 1.2 g intravenous (IV) twice daily, Metronidazole 500 mg three times daily IV, ketoprofen 0.1 g twice daily, enoxaparin 0.4 ml once daily subcutaneous, dexamethasone 8 mg IV once daily. Additionally, drops containing dexamethasone and tobramycin every two hours were used for the left eye. Under general endotracheal anaesthesia, an incision and drainage of the left orbital phlegmon were performed from the supraorbital traumatic wound and suborbital incisions, resulting in abundant purulent exudate. The abscess cavity was rinsed with saline. A flow drain was introduced (Fig. 8). The wounds were surgically prepared and the necrotic masses were removed. In the postoperative period, the level of CRP and WBC was monitored—a decrease in CRP and WBC was observed. A control CT performed on the 3rd day after the procedure showed the correct position of the drain in the eye socket and a significant reduction in exophthalmos. The microbiological examination revealed the alarm pathogen Streptococcus pyogenes susceptible to empirical therapy, Klebsiella pneumoniae, Proteus mirabilis. On the 3rd day after the procedure, the patient reports a subjective sense of light in the left eye (Fig. 9). On the 8th day of hospitalization, the patient was returned to the Ophthalmology Department. The consequence of the injury and infection was permanent blindness of the left eye.
Physical examination shows a contaminated, extensive wound to the skin of the upper eyelid and the left supraorbital area, penetrating the orbital along the roof and the sidewall, from which the exudate of the purulent content emerges. Left eye exophthalmos, the blindness of the left eye, significantly limited mobility of the left eyeball. Due to the swelling, the palpebral fissure was narrowed
Discussion
Owing to the retrospective nature of this study, it was granted an exemption by the Poznan University of Medical Science review board.
The first literature case reports of orbital abscess originated in 1884 [5, 6]. However, PubMed research revealed only 254 results using the formula orbital[title] AND abscess[title], and 863 results, when using the formula orbital[title/abstract] AND abscess[title/abstract] (and 1359 results for orbital[all fields] AND abscess[all fields]).
Orbital abscess formation occur in 8% of patients with retroseptal orbital cellulitis [7].
Symptoms
The most frequently encountered signs and symptoms include periorbital edema, restricted ocular movement, orbital pain, proptosis, periorbital erythrema, chemosis and vision deterioration—Table 1. [3, 8]–[39]
Etiology
Bacterial etiology is the most common and regards pathogenes such as Streptococcus spp. [7, 11, 14, 16, 28, 31, 33, 35, 39, 40], Staphylococcus aureus [9, 36, 40] (also methycylin resistant Staphylococcus aureus [20, 21, 34, 40]) and Pseudomonas aeruginosa [24, 30, 41]. Additionally, wide spectrum of bacteria are rarely encountered: Haemophilus spp. [28, 39], Coagulase-negative staphylococcus [23, 40], Peptostreptococcus spp. [8, 27], Citrobacter freundii [11, 40], Enterobacter spp. [40], Enterococcus spp. [39, 40], Acinetobacter spp. [40], Actinomyces israelii [40], Diphteroids [40], Morganella Morgani [17], Proteus mirabilis [17, 40], Escherichia coli [40], Granulicatella Adiacens [22], Prevotella melaninogenica [27], Eikenella corrodens [28],, Propionibacterium acne [42], Pseudomonas stutzeri [38] as well as polymicrobial infections [3, 11, 28, 39, 40]. Gram-negative infections are at higher risk of visual deterioration or loss, especially in regard to Acinetobacter spp. [40] Fungal etiology occurs very infrequently and includes Exophiala dermatitidis [15] and Candida albicans [11]. Occasionally, the infection etiology remains unknown despite culture sampling and isolation attempt [10, 19, 29, 43]—according to Teena et al. 68.8% of orbit specimens finds the infectious pathogen [40]. Some articles omit stating exact etiology [12, 13, 26].
Pathogenesis
Orbital abscess formation originates from odontogenic, periorbital, sinonasal, traumatic, or systemic pathologies, like wise iatrogenic complications. Odontogenic pathogenesis includes incorrect or complicated intraoral interventions, such as tooth extractions and endodontic treatment [12, 19, 33, 35] as well as delayed dental procedures related to 'extreme phobia' of dental procedures and severe caries [8, 18]. Common ophthalmological procedures may result in orbital abscess: posterior subtendon injection [9, 15, 29, 34], strabismus surgery [16], trabeculectomy [38], canaliculitis surgical treatment [28], or orbital implants placement [3, 42]. Frequently, the abscess arises from dacryocystitis [17, 23, 27, 37, 44, 45], and rarely from concjuctivitis [20]. Another cause come from sinus pathologies such Pott's Puffy Tumor [13] or frontoethmoidal mucopyocele [30] as well as sinusitis and nonspecific upper respiratory infection [20, 46]. The important origin regards posttraumatic fractures, lacerations and impacted foreign bodies [11, 22, 26]. Finally, systemic conditions such as human immunodeficiency virus (HIV) infection [46], immunosuppression after transplantation [24] or congenital immunodeficiency (in pediatric population) [41]. There are cases where exact pathogenesis remains unknown [25, 32].
Sequels
Orbital abscess sequels apply not only to the orbit, restricted ocular motility, impaired or lost vision, and central retinal artery occlusion. Infection may spread causing superior orbital fissure syndrome, cavernous sinus thrombosis, meningitis, brain abscess, and subdural empyema [23, 47]–[49]. On the other hand, Hughes et al. reported a case of an orbital abscess concomitant to aseptic meningitis and cavitory lung lesions which pathogenesis concerned severe caries. They claimed hematogenous spread of the infection, because maxillary sinus showed no infection. [8]
Imaging
Ocular ultrasonography provides immediate assessment of an orbit and opportunity to follow treatment outcomes without unnecessary exposure to radiation [20, 21]. However, more accurate examinations such as CT or MRI are crucial to evaluate local extension and involvement of adjacent structures, especially before surgical treatment. Despite CT is the first line imaging technique in eye infections and pathologies, it has limited power to visualise orbital abscess. In case of severe symptoms and not significant CT examination, additional MRI scans should be performed [21, 25, 50]. According to Sepahdari et al. diffusion-weigted imaging (DWI) of MRI provides accurate imaging of orbital abscess and grants the sufficient tool for patients with renal insufficiency, if used without intravenous contrast. However, they performed a preliminary study with only 9 cases of orbital infections, including 2 lacrimal gland abscess, 2 eyelid abscess, extraconal abscess, intraconal abscess, and subperiosteal abscess [51]. Panoramic radiograph may be used to visualise oral pathologies in case of odontogenic origin of orbital abscess. [31]
Differential Diagnosis
Numerous conditions present similar symptoms as orbital abscess, possibly misleading the diagnosis, for instance: neoplasms—osteoma of the ethmoid sinus, [52], small cell neuroendocrine carcinoma of the orbit [53] plasmacytoma [54], infections—primary orbital tuberculosis [55], globe subluxation [56], or liquefied hydrogel implant accumulation [57]. On the other hand, physicians reported cases of true orbital abscess primarily misdiagnosed with other pathologies, such as retrobulbar haemorrhage [11], tumor [25], fronto-orbital mucocele, [32] or granulomatosis with polyangitis exacerbation [58]. Therefore, precise diagnostic process is crucial, including past medical history, clinical assessment, imaging, microbiological tests and histopathological evaluation.
Treatment
According to current review, surgical treatment was necessary in 94% of cases. Abscess drainage is achieved via multiple approaches depending on its localisation: transculuncular, lateral or anterior orbitotomy, Caldwell-Luc approach, intranasal endoscopy, needle aspiration guided by ulstrasound, lower eyelid incision, subcilliar incisio, incision in four quadrants of the orbit. If it is necessary, surgical debridement of necrotic tissues is performed, as well as enucleation or exenteration. Antibiotic therapy is both, initial and supplementary to surgical treatment. Only two cases resolved with alone antibiotics administration—Table 2 [3, 8]–[28, 30, 32]–[39, 42].
Outcomes
Complete recovery succeed in 49% of cases, whereas 11% of patients recovered with vision loss, 9% with vision deterioration, 6% with persistent movement restrictions, 3% with exenteration, 3% with enucleation, 3% with residual enophatomos, 3% with residual proptosis, and 3% with corneal scarring. Exact results were not presented in 14% of cases. Fortunately, any patient died in the investigated reports [3, 8]–[28, 30, 32]–[39, 42].( Table 3)
References
Krohel GB, Krauss HR, Winnick J (1982) Orbital abscess. Ophthalmology 89(5):492–498. https://doi.org/10.1016/S0161-6420(82)34763-6
Mehrotra MC (1965) Cavernous sinus thrombosis with generalized septicemia. Oral Surg Oral Med Oral Pathol 19(6):715–719. https://doi.org/10.1016/0030-4220(65)90340-3
Kent SS, Kent JS, Allen LH (2012) Porous polyethylene implant associated with orbital cellulitis and intraorbital abscess. Can J Ophthalmol 47(6):e38–e39. https://doi.org/10.1016/j.jcjo.2012.03.043
Chandler JR, Langenbrunner DJ, Stevens ER (1970) ‘The pathogenesis of orbital complications in acute sinusitis. Laryngoscope 80(9):1414–1428. https://doi.org/10.1288/00005537-197009000-00007
Emrys-Jones A (1884) Case of Orbital Abscess Communicating with the Brain. BMJ 1(1208):355–355. https://doi.org/10.1136/bmj.1.1208.355
Lippincott JA (1884) Two cases of orbital abscess. Trans Am Ophthalmol Soc 3:702–707
Van der Veer EG, van der Poel NA, de Win MML, Kloos RJ, Saeed P, Mourits MP (2017) True abscess formation is rare in bacterial orbital cellulitis; consequences for treatment. Am J Otolaryngol 38(2):130–134. https://doi.org/10.1016/j.amjoto.2016.11.006
Hughes E, Wynne N, Quinn S, Fulcher T (2017) Odontogenic orbital abscess with intracranial and pulmonary involvement. Orbit 36(6):459–461. https://doi.org/10.1080/01676830.2017.1337193
Rhatigan M, McAnena L, McElnea E, Connell P, Fulcher T (2017) Orbital abscess following posterior subtenon injection of triamcinolone acetonide. Orbit 36(3):135–136. https://doi.org/10.1080/01676830.2017.1279668
Procacci P, Zangani A, Rossetto A, Rizzini A, Zanette G, Albanese M (2017) Odontogenic orbital abscess: a case report and review of literature. Oral Maxillofac Surg 21(2):271–279. https://doi.org/10.1007/s10006-017-0618-1
Mohammed Saed S, Davies I, Ho MW (2017) Orbital abscess that masqueraded as a retrobulbar haemorrhage. Br J Oral Maxillofac Surg 55(3):334–335. https://doi.org/10.1016/j.bjoms.2016.09.009
Arora N, Juneja R, Meher R (2018) Complication of an odontogenic infection to an orbital abscess: the role of a medical fraudster (“Quack”). Iran J Otorhinolaryngol 30(98):181–184
Linton S, Pearman A, Joganathan V, Karagama Y (2019) Orbital abscess as a complication of Pott’s puffy tumour in an adolescent male. BMJ Case Rep 12(7):e229664. https://doi.org/10.1136/bcr-2019-229664
Wang Y, Zhang J, Dong L, Jiang H, Song X (2019) Orbital abscess treated by ultrasound-guided fine needle aspiration and catheter drainage: a case report. Medicine (Baltimore) 98(39):e17365. https://doi.org/10.1097/MD.0000000000017365
Iwahashi C et al (2020) Orbital abscess caused by Exophiala dermatitidis following posterior subtenon injection of triamcinolone acetonide: a case report and a review of literature related to exophiala eye infections. BMC Infect Dis 20(1):566. https://doi.org/10.1186/s12879-020-05294-y
Strul S, McCracken MS, Cunin K (2014) Orbital cellulitis and intraconal abscess formation after strabismus surgery in an adult patient. J Am Assoc Pediatr Ophthalmol Strabismus 18(1):82–84. https://doi.org/10.1016/j.jaapos.2013.09.011
Carruth BP, Wladis EJ (2013) Orbital abscess from dacryocystitis caused by morganella morganii. Orbit 32(1):39–41. https://doi.org/10.3109/01676830.2012.736598
Vijayan A, Sreejith V, Lnu R, Ahamed G (2012) Orbital abscess arising from an odontogenic infection. J Contemp Dent Pract 13(5):740–743. https://doi.org/10.5005/jp-journals-10024-1220
de Medeiros EHP, Pepato AO, Sverzut CE, Trivellato AE (2012) Orbital abscess during endodontic treatment: a case report. J Endod 38(11):1541–1543. https://doi.org/10.1016/j.joen.2012.06.039
Secko M, Romney M-L, Gullett J (2012) Sonographic diagnosis of a retro-orbital abscess. J Ultrasound Med 31(7):1137–1137. https://doi.org/10.7863/jum.2012.31.7.1137
Derr C, Shah A (2012) Bedside ultrasound in the diagnosis of orbital cellulitis and orbital abscess. Emerg Radiol 19(3):265–267. https://doi.org/10.1007/s10140-011-0993-0
Teo L, Looi A, Seah LL (2011) An unusual causative agent for an orbital abscess: granulicatella adiacens. Orbit 30(3):162–164. https://doi.org/10.3109/01676830.2011.569631
Coşkun M et al (2011) Central retinal artery occlusion secondary to orbital cellulitis and abscess following dacryocystitis. Eur J Ophthalmol 21(5):649–652. https://doi.org/10.5301/EJO.2011.6493
Hull S, Mace AD, Lalchan S-A, Saleh HA, Olver JM (2011) ‘Orbital floor abscess secondary to sinusitis in an immunocompromised patient.’ ophthal Plast Reconstr Surg 27(5):e139–e141. https://doi.org/10.1097/IOP.0b013e318207120e
Qi D, He W (2010) ‘Orbital abscess caused by viridans streptococcus.’ Ophthal Plast Reconstr Surg 26(6):500–501. https://doi.org/10.1097/IOP.0b013e3181cf94b3
Serra ECS, Sverzut CE, Trivellato AE (2009) Orbital abscess after facial trauma. Braz Dent J 20(4):341–346. https://doi.org/10.1590/S0103-64402009000400014
MC Martins, JR da, S Ricardo, PMS Akaishi, AAV. e Cruz, ‘Orbital abscess secondary to acute dacryocystitis: case report’, Arq. Bras. Oftalmol., 71(4):576–578, doi: https://doi.org/10.1590/S0004-27492008000400020.
Hatton MP, Durand ML (2008) ‘Orbital cellulitis with abscess formation following surgical treatment of canaliculitis.’ Ophthal Plast Reconstr Surg 24(4):314–316. https://doi.org/10.1097/IOP.0b013e31817e9be7
Ram J, Ichhpujani P, Gupta A, Sukhija J, Dogra M (2008) Acute orbital abscess complicating deep posterior subtenon triamcinolone injection. Indian J Ophthalmol 56(3):246. https://doi.org/10.4103/0301-4738.40370
Kau H-C et al (2007) ‘Benign fibrous histiocytoma associated with a frontoethmoidal mucopyocele and orbital abscess.’ Ophthal Plast Reconstr Surg 23(3):236–238. https://doi.org/10.1097/IOP.0b013e31803ecf24
I-K Kim, J-R Kim, K-S Jang, Y-S Moon, S-W Park (2007) ‘Orbital abscess from an odontogenic infection’, Oral Surg Oral Med Oral Pathol Oral Radiol Endodontology,103(1):1–6, https://doi.org/10.1016/j.tripleo.2006.07.002.
Aydin E, Akkuzu G, Akkuzu B, Bilezikci B (2006) Frontal mucocele with an accompanying orbital abscess mimicking a fronto-orbital mucocele: case report. BMC Ear Nose Throat Disord 6(1):6. https://doi.org/10.1186/1472-6815-6-6
Sakkas N, Schoen R, Schmelzeisen R (2007) Orbital abscess after extraction of a maxillary wisdom tooth. Br J Oral Maxillofac Surg 45(3):245–246. https://doi.org/10.1016/j.bjoms.2005.09.010
Engelman CJ (2004) Orbital abscess following subtenon triamcinolone injection. Arch Ophthalmol 122(4):654. https://doi.org/10.1001/archopht.122.4.654
N Zachariades, E Vairaktaris, M Mezitis, G Rallis, C Kokkinis, M Moschos (2005) ‘Orbital abscess: Visual loss following extraction of a tooth—Case report’, Oral Surg Oral Med Oral Pathol Oral Radiol Endodontology,100(4):70–73, https://doi.org/10.1016/j.tripleo.2005.02.062.
Irvine F, McNab AA (2002) Orbital abscess following uncomplicated phacoemulsification cataract surgery. Clin Experiment Ophthalmol 30(6):430–431. https://doi.org/10.1046/j.1442-9071.2002.00574.x
Ataullah S, Sloan B (2002) Acute dacryocystitis presenting as an orbital abscess. Clin Experiment Ophthalmol 30(1):44–46. https://doi.org/10.1046/j.1442-9071.2002.00476.x
Lebowitz D, Gürses-Ozden R, Rothman RF, Liebmann JM, Tello C, Ritch R (1960) Late-onset bleb-related panophthalmitis with orbital abscess caused by pseudomonas stutzeri. Arch Ophthalmol Chic Ill 119(11):1723–1725
Papesch ME (2000) Radiology case report: a nasty orbital abscess. Emerg Med J 17(6):431–431. https://doi.org/10.1136/emj.17.6.431
Teena M, Mary J, Suneetha N, Usha V (2012) Microbiological profile of orbital abscess. Indian J Med Microbiol 30(3):317. https://doi.org/10.4103/0255-0857.99494
Rosser A, Modha DE (2015) Pseudomonas aeruginosa retro-orbital abscess and cerebritis leading to a diagnosis of interleukin-1 receptor-associated kinase-4 deficiency. J Microbiol Immunol Infect 48(1):119–120. https://doi.org/10.1016/j.jmii.2013.09.009
Hong SW, Paik J-S, Kim S-Y, Yang S-W (2006) A case of orbital abscess following porous orbital implant infection. Korean J Ophthalmol 20(4):234. https://doi.org/10.3341/kjo.2006.20.4.234
Pushker N et al (2009) ‘Orbital abscess with unusual features.’ Plast Reconstr Surg 25(6):450–454. https://doi.org/10.1097/IOP.0b013e3181b80b27
Maheshwari R, Maheshwari S, Shah T (2009) Acute dacryocystitis causing orbital cellulitis and abscess. Orbit 28(2–3):196–199. https://doi.org/10.1080/01676830902925529
Kikkawa DO, Heinz GW, Martin RT, Nunery WN (1960) AS Eiseman (2002) ‘Orbital cellulitis and abscess secondary to dacryocystitis.’ Arch. Ophthalmol Chic Ill 120(8):1096–1099
Grüter BE, Pangalu A, Landau K, Wichmann W (2017) Orbital cellulitis with apparent thrombosis of the left cavernous sinus and perioptical abscess formation. Clin Neuroradiol 27(3):379–382. https://doi.org/10.1007/s00062-017-0563-2
Suneetha N, Battu RR, Thomas RK, Bosco A (2000) Orbital abscess: management and outcome. Indian J Ophthalmol 48(2):129–134
Ogundiya DA, Keith DA, Mirowski J (1989) Cavernous sinus thrombosis and blindness as complications of an odontogenic infection: report of a case and review of literature. J Oral Maxillofac Surg 47(12):1317–1321. https://doi.org/10.1016/0278-2391(89)90733-7
Allan BP, Egbert MA, Myall RWT (1991) Orbital abscess of odontogenic origin. case report and review of the literature. Int J Oral Maxillofac Surg 20(5):268–270. https://doi.org/10.1016/S0901-5027(05)80150-X
Mcintosh D, Mahadevan M (2008) Failure of contrast enhanced computed tomography scans to identify an orbital abscess. the benefit of magnetic resonance imaging. J Laryngol Otol 122(6):639–640. https://doi.org/10.1017/S0022215107000102
Sepahdari AR et al (2009) MRI of orbital cellulitis and orbital abscess: the role of diffusion-weighted imaging. Am J Roentgenol 193(3):W244–W250. https://doi.org/10.2214/AJR.08.1838
S Lee, JR. Mallen, WH. Ehlers, TE Falcone(2020) ‘Large Ethmoid Sinus Osteoma Presenting as Vision Threatening Orbital Abscess’, Ear. Nose. Throat J., p. 014556132093195, doi: https://doi.org/10.1177/0145561320931950.
Mittal R, Kaza H, Agarwal S, Rath S, Gowrishankar S (2019) Small cell neuroendocrine carcinoma of the orbit presenting as an orbital abscess in a young female. Saudi J Ophthalmol 33(3):308–311. https://doi.org/10.1016/j.sjopt.2018.07.003
Russell DJ, Seiff SR (2017) ‘Orbital plasmacytoma mimicking an orbital abscess.’ Ophthal Plast Reconstr Surg 33(2):e32–e33. https://doi.org/10.1097/IOP.0000000000000685
Yoon HS, Na YC, Lee HM (2019) Primary orbital tuberculosis on the lower eyelid with cold abscess. Arch Craniofacial Surg 20(4):274–278. https://doi.org/10.7181/acfs.2019.00339
Mylvaganam H, Goodglick T (2017) Orbital “pseudo-abscess” in a patient with spontaneous subluxation of globe: a case report. Am J Ophthalmol Case Rep 7:20–22. https://doi.org/10.1016/j.ajoc.2017.04.007
Pakdel F, Hadizadeh H, Pirmarzdashty N, Kiavash V (2015) Masquerading orbital abscess following attempted hydrogel scleral buckle removal: diagnostic value of orbital magnetic resonance spectroscopy. Orbit 34(4):179–182. https://doi.org/10.3109/01676830.2015.1014516
de Silva DJ, Cole C, Luthert P, Olver JM (2007) Masked orbital abscess in Wegener’s granulomatosis. Eye 21(2):246–248. https://doi.org/10.1038/sj.eye.6702211
H. Gavriel (2010) ‘Management implications of diagnosing orbital abscess as subperiosteal orbital abscess’, Rhinol. J, 48(1), doi: https://doi.org/10.4193/Rhin09.090.
Eviatar E, Kessler A, Pitaro K (sss2009) Bidirectional orbital approach enhances orbital abscess drainage. Rhinol J 47(3):293–296. https://doi.org/10.4193/Rhin08.215
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the publication.
Corresponding author
Ethics declarations
Conflict of interest
The author declare that they have no conflict of interest.
Ethical Approval
Ethical approval was not necessary for the preparation of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zawadzki, T., Komisarek, O., Pawłowski, J. et al. Orbital Abscess—Two Case Reports with Review. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2), 1334–1343 (2022). https://doi.org/10.1007/s12070-021-02486-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02486-z