16 Esophagus
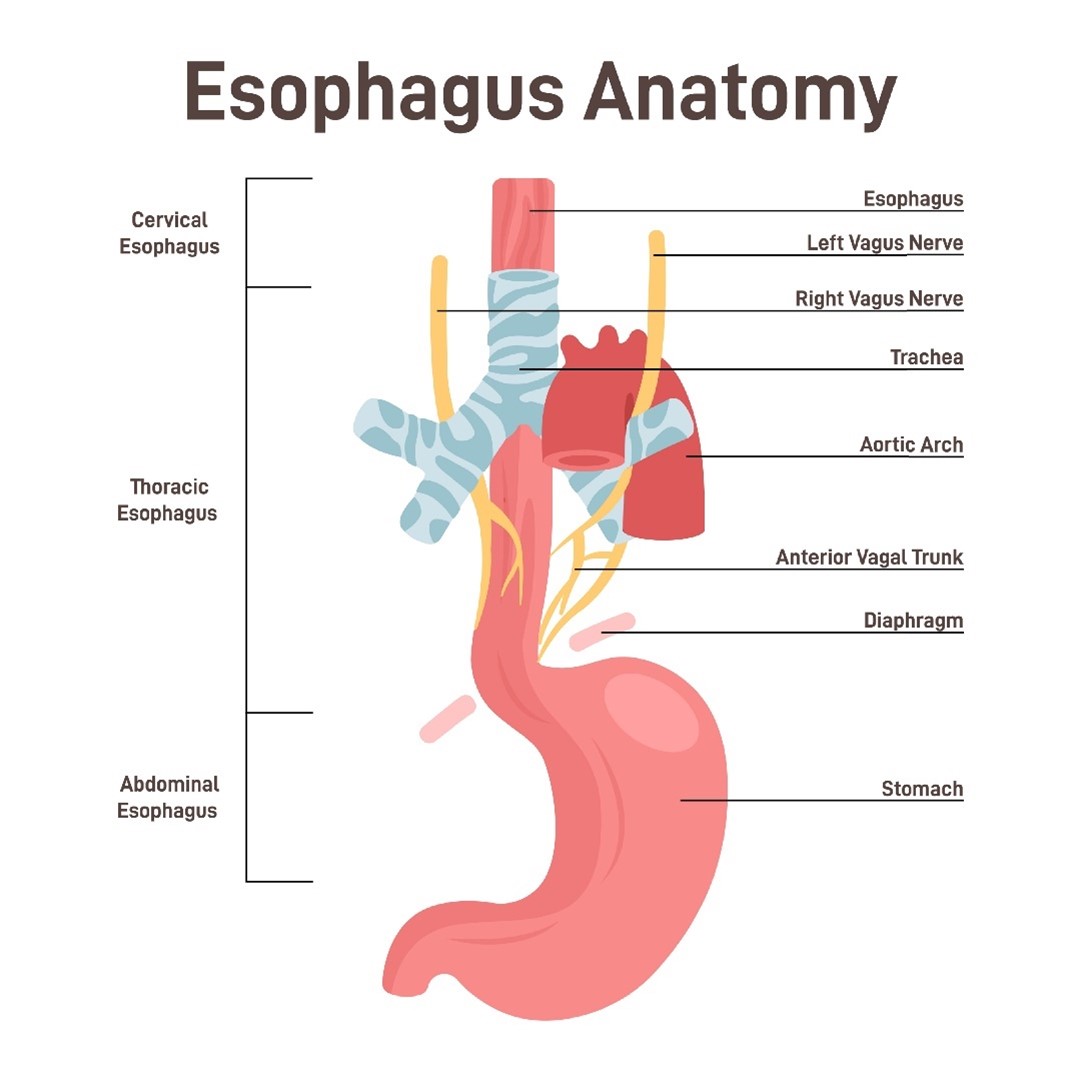
The esophagus is a muscular tube anterior to the spine and posterior to the trachea that connects the cricoid cartilage of the pharynx to the stomach at the gastroesophageal (GE) junction. It is divided into three sections: cervical, middle, and lower. Esophageal cancer is a rare form of cancer, accounting for only 1% of all new cancer cases in the US. About 4 out of 5 people diagnosed with esophageal cancer are male, and the average age at diagnosis is 67.
Several factors contribute to the development of esophageal cancer. These include smoking, excessive alcohol consumption, gastroesophageal reflux disease (GERD), and Barrett’s Esophagus. Two common types of esophageal cancer are squamous cell carcinomas and adenocarcinomas.
- Squamous cell carcinoma is often associated with tobacco and alcohol abuse and typically occurs in the upper two-thirds of the esophagus.
- Adenocarcinomas of the esophagus tend to present in the lower one-third of the esophagus, where the distal esophagus meets the proximal stomach at the GE junction. These cancers are primarily linked to GERD and Barrett’s esophagus. The squamous cells typical of the distal esophagus transform (metaplasia) into columnar epithelial cells, which are better able to tolerate the acidic conditions known as Barrett’s Esophagus. The change in tissue type is responsible for the cancers being classified as adenocarcinomas.
Unlike many other organs, the esophagus lacks a serosal layer and instead has adventitia, a fibrous connective tissue. The adventitia has a rich lymphatic supply, which contributes to the early spread of these cancers and a poor prognosis.
Patient Simulation & Special Considerations: Esophagus
When simulating a patient for an esophagus treatment, a supine position is used, and it is essential to consider which portion of the esophagus has cancer.
- For the upper esophagus, use a head and shoulder mask and a headrest that extends up the mandible to reduce its dose.
- For the lower two-thirds of the esophagus, the arms are above the patient’s head in an arm board or vacloc. The doctor may request patients not eat 2-4 hours before simulation and daily treatment to aid in reproducibility. Educate the patient on the importance of this and ask them daily before treatment.
Straightening the patient’s body from SSN to xiphoid and umbilicus is vital, especially when treating the distal esophagus. Localization marks are placed anteriorly along the patient’s midline and lateral marks on each side. Scan parameters extend from around the EAM (external auditory meatus) to about the second lumbar vertebra.
Treatment Volume Localization: Esophagus
Esophageal cancers tend to spread via the lymph. Skip metastasis are a particular pattern of lymph node spread involving the distant lymph nodes from the tumor site but not the peritumoral lymph nodes. As such, longitudinal treatment boarders are generous; the PTV is typically 5 cm superior/inferior beyond the treatment volume. Anterior straightening marks are important to account for the long treatment fields. The lateral margins are generally 2-2.5 cm beyond demonstratable disease. Motion management 4D techniques previously described may be beneficial for tumors of the distal esophagus that move with the diaphragm.
Treatments of the esophagus are often given definitively or preoperatively and in combination with chemotherapy. In patients receiving concurrent chemo, slightly lower doses are sometimes used to prevent toxicities. Patients with positive surgical margins or regional nodal involvement can receive treatment postoperatively. Palliative treatment is beneficial in relieving symptoms of obstruction and dysphagia.
|
Organs at Risk (OARs)
|
TD 5/5 (Whole Organ)
|
Outcome Associated
|
|
Spinal Cord
|
45 or 47 Gy
|
Myelitis/Necrosis
|
|
Lung
|
18 Gy
|
Pneumonitis
|
|
Heart
|
40 Gy
|
Pericarditis
|
|
Esophagus
|
55 Gy
|
Stricture/perforation
|
|
Brachial plexus
|
60 Gy
|
Nerve damage
|
|
Liver
|
30 Gy
|
Clinical hepatitis
|
|
Kidney
|
23 Gy
|
Nephritis/Loss of function
|
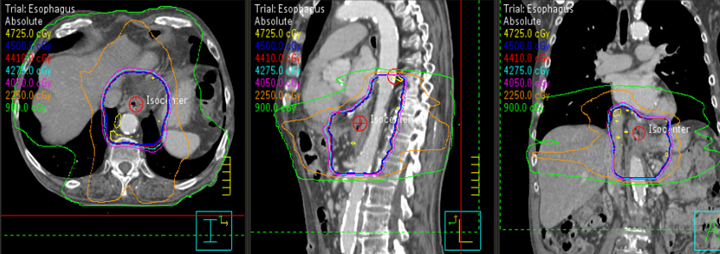
Treatment Techniques: Esophagus
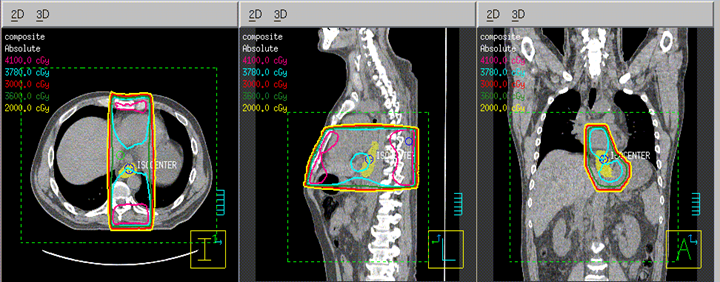
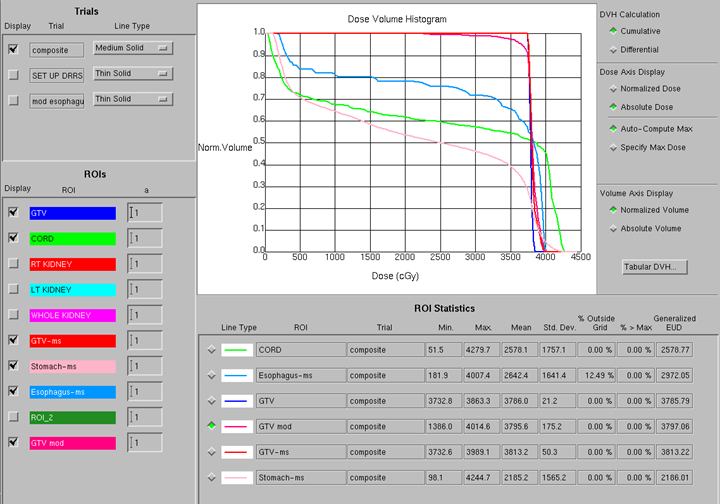
Treatment techniques include 3D conformal radiation therapy (3DCRT) using multiple beam angles, or IMRT. When comparing the two, IMRT can often reduce the dose to critical structures while delivering the prescribed dose to the primary tumor and areas at risk. Higher energy beams (10 MV) minimize the dose delivered to the lung volume. Treating the supraclavicular lymph nodes is considered for the upper two-thirds of the esophagus to 45 Gy.
- Image Guided Radiation Therapy (IGRT): Image guidance uses daily imaging in the localization and treatment of cancer. Imaging modalities include CT, MR, and kV & MV images. In general, when aligning images, align to the planning target volume (PTV) and verify the position of the spine and carina.
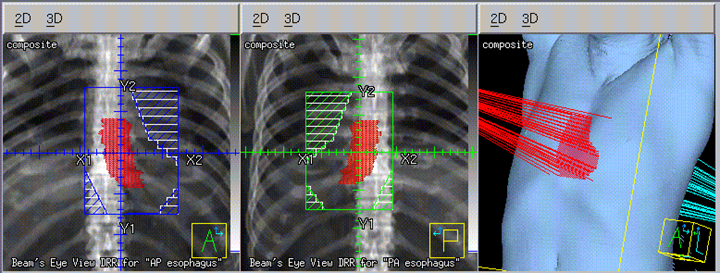
- 3D-CRT (Computerized Radiotherapy): Uses multi-leaf collimators (MLC) to conform each beam shape to the PTV. The size of the PTV and its proximity to critical structures dictate the beam arrangement/angles. With increasing disease stage, more beam angles are added to improve the overall dose to the tumor and reduce the cumulative dose to the lung volume and other OARs. Treatments of the upper one-third of the esophagus are more complicated due to the curvature of the spine and the angle of the esophagus. Anterior oblique wedged fields should be carefully planned to exclude the spinal cord and wedges may be necessary for dose uniformity. For the lower two-thirds of the esophagus, AP/PA treatments to the spine tolerance of 45 Gy are delivered. A boost is often delivered with a cord-sparing technique and custom beam shaping to minimize the dose to normal lung tissue.
- Three-field: Anterior and two posterior oblique fields (with wedges) can reduce the spinal cord dose
- Four-field: Two anterior and two posterior oblique fields minimize the dose to the spinal cord
- Multiple-field: 5-7+ conformal beams target the PTV
- Volumetric Modulated Arc Therapy (VMAT)/Intensity Modulated Radiation Therapy (IMRT): VMAT/IMRT plans significantly reduce the dose to normal tissues and increase dose conformity to the PTV. An arc technique is best for complex treatments of the upper esophagus. These treatments often utilize dynamic treatment techniques. It is essential to be aware that as the beam moves around the patient, the target’s and spinal cord’s shape and position change in the Beam’s Eye View.
|
Definitive Chemoradiation
|
50-50.4 Gy in 25-28 daily fractions with cisplatin-5FU*
|
45-50.4 Gy in 25-28 daily fractions if radiation is given preoperatively*
|
|
Curative Radiation Alone
|
55 Gy in 20 daily fractions of 2.75 Gy given in 4 weeks*
|
60-65 Gy using IMRT/VMAT or off-cord bst after 45 Gy
|
|
Palliative Radiation
|
30 Gy in 10 fractions (3 Gy/fx)
|
20 Gy in 5 fractions (4 Gy/fx)
|
Media Attributions
- eso anatomy © inspiring.team is licensed under a All Rights Reserved license
- eso 2 field © University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- eso 2 field isodose
- eso 2 field dvh © University of Iowa Radiation Therapy Program
- eso VMAT isodose © University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
When one type of mature tissue is replaced by another type of mature tissue not typically found there
The outermost layer of connective tissue surrounding an organ or vessel
A common metastatic pattern in NSCLC occurring when lateral lymph nodes have disease without involvement in the central lymph nodes

