Pseudomonas Otitis
Susan Paterson, VetMB, MA, DVD, DECVD, FRCVS, Virtual Vet Derms, Kendal, United Kingdom

Profile
Definition
Pseudomonas otitis results from infection with the gram-negative bacillus Pseudomonas aeruginosa. It is a common cause of chronic otitis in dogs but rarely causes otitis in cats. Infection with Pseudomonas is recognized as being a perpetuating factor in otitis externa; therefore, identifying an underlying cause for the disease is just as important as diagnosis and treatment.
Pathophysiology
The pathophysiologic changes that occur in chronic otitis predispose the animal to Pseudomonas infection. Inflammation itself does not lead to infection. In acute disease, dermal edema, altered barrier function, and changes in cerumen composition lead to increased numbers of bacteria in the ear canal, typically creating a shift toward coagulase-positive staphylococci.1
As the disease becomes chronic, the otic epithelium changes from a thin layer of migrating cells to hyperplastic, stratified, squamous epithelium. Epithelial migration halts, leading to an accumulation of debris within the lumen. Hyperplasia of glandular tissue ensues, narrowing the lumen and leading to increased humidity and pH within the canal—environmental changes conducive to gram-negative bacterial infection, especially with Pseudomonas species.2
Breed Predisposition
The cocker spaniel is predisposed to Pseudomonas infections because its physiologic response to inflammatory stimuli differs from that of other breeds. Their ear canals contain compound (rather than simple) hair follicles that are densely arranged, and they respond to chronic inflammation by marked ceruminous gland hyperplasia rather than by fibrosis. These 2 factors create a narrow, hairy, humid canal that is ideal for Pseudomonas infection.2
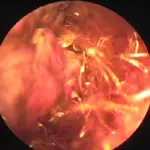
Severely ulcerated ear canal in dog with Pseudomonas infection

Ulcerated ear in cocker spaniel with Pseudomonas infection
Clinical Signs
Pseudomonas otitis:
Painful, not pruritic
Usually unilateral
Yellow/green malodorous suppurative mucoid discharge
Severe inflammation and ulceration of the canal (Figures 1 and 2)
Otitis media (~83% of cases of chronic disease1)
Otitis media commonly presents with signs of:
Head shaking
Pain on palpation of the ear pinna
Discomfort on opening the jaw
Occasional neurologic signs, including: Horner’s syndrome, facial nerve paralysis, keratoconjunctivitis sicca
Otitis: Primary & Predisposing Factors
Pseudomonas infection is almost always a secondary cause of otitis. To prevent recurrence of the disease after therapy, the underlying disease must be identified and managed.
The most common primary factors associated with disease include allergy (atopy), endocrine disease (hypothyroidism), and keratinization disorders.
Important predisposing factors primarily relate to the anatomic features of the ear, such as hairy ear canals and pendulous pinnae.
Diagnosis
Diagnosis can usually be made on the basis of the characteristic clinical signs, but confirmatory diagnostic tests should still be performed to determine appropriate therapy.
Cytology Sample Collection
Collect a sample of discharge by inserting a cotton-tipped applicator through a disinfected otoscope cone positioned near the horizontal canal.
Extend the swab beyond the end of the cone and wipe firmly along the otic epithelium.
Aim to sample the horizontal canal, not the vertical one, to avoid contamination with commensal organisms.
Roll the swab onto a slide, heat fix, and stain with a modified Wright’s-Giemsa stain.
Evaluate for bacteria (cocci and rods), yeast (Malassezia pachydermatis), and inflammatory cells.
Interpretation
Increased numbers of bacteria in the presence of neutrophils suggest bacterial infection. Pseudomonas appears as rod-shaped organisms (Figure 3); if rods are identified, a second swab should be taken from the same site for submission for culture and sensitivity due to the potential for resistant bacteria. If otitis media is present, an additional sample should be taken from the middle ear because the susceptibility pattern of organisms from the 2 locations can be different.3
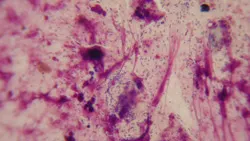
Cytology from ear with Pseudomonas infection
Samples from Middle Ear
When the eardrum is ruptured, a sample can be collected using a sterile swab or a syringe attached to a urinary catheter inserted into the bulla. In the latter case, 0.5 mL of sterile saline may be instilled into and subsequently suctioned out of the tympanic bulla to collect a sample.
If the tympanic membrane is intact, a myringotomy can be performed by inserting a urinary catheter (with a sharpened end) through the caudo-ventral quadrant of the pars tensa. Sterile saline can be instilled and suctioned as previously described.
Imaging & Hearing Tests
Computed tomography (CT) (Figure 4) and magnetic resonance imaging (MRI) are preferable to radiography, which is an insensitive means of diagnosing otitis media. Brainstem auditory evoked response (BAER) testing is an accurate method of assessing hearing (Figure 5). When chronic irreversible change is present in the canals (calcification of the soft tissue) or middle ear (granulation tissue or bony change present in the bulla), or when the animal is deaf, medical therapy is inappropriate and a total ear canal ablation with bulla osteotomy should be performed.
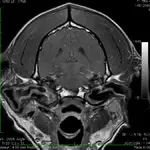
Transverse plane T1-weighted postcontrast image in a 3-year-old dog with bilateral otitis media and otitis externa. The lining of the bullae and the walls of the external ear canals are enhanced, consistent with inflammation and exudate in the bullae.
Treatment
Inpatient or Outpatient
Ear cleaning is the first and most important therapeutic step. Thorough cleaning of the ear canal and middle ear is essential and can be achieved only in an anesthetized and intubated animal in the clinic. Subsequent therapy may be undertaken by the client on an outpatient basis.
Ear Cleaning
Water should be used as the first flush to break up mucus from the middle ear, followed by an antiseptic flush. Any product that lowers the pH of the ear canal will be effective in killing Pseudomonas; however, acetic acid at a concentration of 2% is lethal to the organism within 1 minute of contact and can be used daily to flush the ear canal before applying a topical antibiotic solution.4,5 This strategy appears to be very safe even if the eardrum is ruptured.
Where resistant infections are known to be present, a second antiseptic solution, trisaminomethane ethylenediaminetetraacetic acid (Tris EDTA), may be used as a final rinse that is not flushed away.6 Used as a prepared solution or in combination with other topical products (eg, chlorhexidine or ketoconazole), Tris EDTA increases the permeability of the Pseudomonas cell membrane by binding calcium and magnesium ions. A Tris EDTA flush should be used twice daily prior to antibiotic administration.
Topical Medication
Topical Antibiotics
Initial selection of topical therapy may be made empirically but can be changed after culture results are obtained. Good first-line drugs include gentamicin or a fluoroquinolone, such as enrofloxacin or marbofloxacin. Veterinary ear drops containing these antibiotics are not safe for use in the middle ear and should only be instilled if the eardrum can be visualized and is intact; however, aqueous solutions of these antibiotics, as well as silver sulphadiazine cream (which can be diluted with sterile water), have been used off-label and are reported to be safe even if the eardrum is ruptured.7
Other antibiotics that may be considered include amikacin, tobramycin, and ticarcillin. These products all have ototoxic potential7 and should only be used when other safer products are deemed unsuitable. They may be mixed with Tris EDTA as a potentiating agent.
Topical Glucocorticoids
Glucocorticoids, such as dexamethasone and betamethasone, help decrease inflammation and reduce exudate from the external ear canal and the bulla. Aqueous solutions of glucocorticoids are considered safe within the middle ear.7 Glucocorticoids can be added to antibiotic solutions and administered after the disinfectant flushes.
Systemic Medication
Systemic Antibiotics
This component of therapy is rarely required and is indicated only when the otitis is poorly responsive to topical treatment. Systemic drug therapy should be based on culture and sensitivity, but enrofloxacin (12–15 mg/kg Q 24 H) or marbofloxacin (5 mg/kg Q 24 H)8 can be used pending culture results.
Systemic Glucocorticoids
An antiinflammatory dose of dexamethasone (0.1 mg/kg) should be given intravenously at the time of the initial ear flush. Systemic glucocorticoids can be used if the otitis is poorly responsive to topical therapy. Methylprednisolone or prednisolone (1.0–1.5 mg/kg Q 24 H) may be used for 5 days, then tapered to an alternate-day regimen until inflammation has resolved.
Length of Therapy
Treatment for chronic Pseudomonas otitis is typically required for at least 4 weeks and may last as long as 3 months. Therapy should be continued until the inflammation in the canals and the middle ear has resolved and cytology of the otic discharge appears normal.
Therapy at a Glance
Cleaning solutions should be used twice daily
Initial flush: Acetic acid 2% followed by Tris EDTA
Dilute topical antibiotics in 12 mL Tris EDTA; instill 0.5 mL into ear Q 12 H after flush*
-Gentamicin
1 mL(4 mg/mL) solution
-Enrofloxacin
4 mL2% solution
-Marbofloxacin
4 mL1% solution
*Alternately, 4 mL topical dexamethasone (2 mg/mL) may be used in place of 4 mL of Tris EDTA.
Follow-Up
Patient Monitoring
After recovery from severe ear disease, the patient should be reevaluated at regular intervals every few months. Owners should be taught effective ear cleaning techniques and how to spot the earliest signs of recurrence. Suitable ear flushes for maintenance therapy include those containing acetic acid or Tris EDTA. Rechecks should involve otoscopic and cytologic assessment.
Prevention
Preventing recurrence of otitis depends on the determination and control of the primary and underlying causes of ear disease. Allergies, especially atopic dermatitis or adverse food reaction, are considered the most common underlying causes of disease. Less common causes include endocrine disorders, keratinization disorders, parasites, and neoplasia.