A good hair day can make you feel like a million bucks, but a bad one can do the opposite. Between bumps on your scalp, frizziness, hair loss, unruly strands, dandruff and more, so much can go wrong that it's a wonder our hair ever looks good!
Fortunately, evidence from the National Institutes of Health shows that a healthy scalp helps produce healthy hair. And as a dermatologist who has treated all of the scalp conditions listed below, I know that when the scalp is unhealthy, it can lead to itchy, uncomfortable rashes, bumps, flakes and even hair loss, as well as sores, red spots and scabs. If you're experiencing unpleasant scalp issues, use this guide to help figure out if you might be suffering from one of these ten common scalp conditions and if so, the best ways to treat them.
The Anatomy of the scalp
The skin on the scalp is different than that on the rest of the body: Besides the obvious profusion of hair follicles, the scalp has more sebaceous glands — teensy glands found in hair follicles (and some hairless parts of the body as well) that release sebum, an oily substance that acts as a lubricant for hair and skin. That makes the scalp a particularly rich environment for microbes, which can bring on various problems — including some that require medical attention. Since it’s nearly impossible to get a good look at the top or back of your own head, it's a great idea to check in with a board-certified dermatologist for a thorough evaluation of your scalp and to come up with a treatment plan that will support a healthy head of hair.
Common scalp conditions (with photos):
Head lice
These tiny insects live in the hair on people’s heads (including eyebrows and eyelashes!) and feed on human blood. While they don’t spread any diseases and they can’t jump or fly, lice can crawl from one person to another if they touch, according to the Centers for Disease Control and Prevention (CDC). When a person is allergic to a lice bite, it can cause itchiness.
What it looks like: Lice eggs (nits) are usually attached to the hair shaft and may be confused with scabs or dandruff flakes. Adult lice are about the size of a sesame seed and tan or gray in color; they may appear darker on darker hair. There may be sores on the scalp if the person’s been scratching.
The causes:
- Usually lice are spread when one person’s head touches another person’s — young kids are the biggest culprits. That said, a lice infestation does not mean a person is dirty.
- It’s also possible — but not likely — to get lice from shared items like clothes, pillows or combs.
The treatments:
- Head lice can usually be taken care of with an OTC shampoo treatment and a lice comb.
- If that doesn’t work, a doctor can prescribe additional medications.
- It’s also smart to vacuum, wash the infected person’s clothes and bedding and disinfect their combs and brushes, according to the CDC.
Lichen Planus
Lichen planus (LP) is an inflammatory disorder that affects the skin and mucus membranes. Research shows it’s common and can show up nearly anywhere on the body, including the mouth, genitals, nails, legs and the scalp (just to name a few spots!).
What it looks like: small purple or red irritated bumps on the scalpand in some cases, hair loss. It can manifest differently on other parts of the body, according to the American Academy of Dermatology (AAD).
The causes:
No one is exactly sure what causes a person to develop LP, but the AAD says these are some likely triggers:
- In rare instances, metal dental fillings have been linked with LP.
- People with Hepatitis C are more likely to have LP.
- Certain medications seem to spark the development of LP so it’s important to tell your dermatologist about everything that you take.
- Genetics may also come into play — one particular type of LP called bullous lichen planus tends to run in families.
The treatments:
- Topicals like corticosteroid, retinoic acid, tacrolimus ointment and pimecrolimus cream can be applied to skin where there are LP lesions.
- Antihistamines and retinoic acid can be taken in pill form.
- Using PUVA therapy, patients either soak parts of their skin in water that contains psoralens (plant compounds that make skin more sensitive to UVA rays) or they take psoralens orally. Then, affected skin is exposed to ultraviolet A (UVA) light.
Seborrheic Dermatitis (Dandruff)
Seb derm, as most derms call it, is one of the most common scalp conditions. In babies, it's called cradle cap; in adults, it causes red, itchy patches with greasy scale or flakes. People usually refer to it as dandruff when it's on the scalp, but seb derm when it affects the face, nose, eyebrows, ears or chest. Research estimates that half of all adults in the world have dandruff so if you're struggling with it you're definitely not alone. Seb derm often comes and goes with triggers such as stress and seasonal changes — it is usually worse in winter and early spring. It's often best to treat seborrheic dermatitis early and aggressively to avoid complications such as hair loss.
What it looks like: greasy scale and dandruff flakes
The causes:
- A yeast (fungus) called malassezia. which is in the oil secretion on the skin, it thought to be the culprit, though doctors aren't certain that this is the cause.
- Parkinson's, depression, diabetes, a weakened immune system and obesity may make a person more likely to have seb derm. So can recovering from a stressful health event, like a heart attack.
- Dry skin can result in flakes as can a sensitivity to certain hair products so it's helpful to look at your scalp care regimen to see if something other than a fungus is causing your flakes.
The treatments:
- A prescription strength anti-yeast shampoo called ketoconazole can help. Since it can be very drying to the hair, Yolanda Lenzy, M.D., board-certified dermatologist and author of Getting to the Root: A Dermatologist's Guide to Understanding Hair, recommends applying the shampoo directly to your scalp 5 to 10 minutes before wetting the hair and then lathering only the scalp area before you rinse it off. "Follow with a moisturizing shampoo and conditioner on the hair shaft to prevent the dryness that Rx shampoos can often cause, especially in more coily hair types," advises Dr. Lenzy.
- OTC shampoos or lotions that contain zinc pyrithione, ketoconazole or sulfur may also help.
- A topical steroid may be prescribed if the shampoo doesn't work, or in combination with the shampoo if the scales are very dense.
Psoriasis
This condition affects about 1 to 2% of the general population and anyone can get it, at any age. Psoriasis can appear on any part of the body, but according to the National Psoriasis Foundation, as many as 45% to 56% of those with psoriasis have it on their scalp. And that kind is one of the most difficult types to treat, according to Seemal Desai, M.D., F.A.A.D., clinical assistant professor in the Department of Dermatology at the University of Texas Southwestern Medical Center. One way to distinguish it from dandruff: The buildup of skin cells creates scaly, patches that are dry, rather than oily. And those patches can itch, hurt, crust up and bleed.
What it looks like: pink plaques with a silvery scale. On darker skin tones, the plaques may be dark red or purplish.
The causes:
- Psoraisis thought to be an immune dysregulation around skin cells that causes the cells in the top layer of skin to go into overdrive.
- Stress can make the situation worse, because it causes an increase in the hormone cortisol, which in turn can boost inflammation.
The treatments:
- Topical steroids, which control the inflammatory response, are the the most common treatment.
- Injections called biologics that help suppress what's causing the flare-ups in tougher cases.
- An excimer laser can work on individual spots that are not responding to other therapies.
- A gentler hair routine can also help, points out Dr. Desai. Not shampooing your hair every day may lessen the amount of skin rashes, or a therapeutic oil cream can also do wonders.
Folliculitis
Folliculitis, a common skin condition, is basically inflammation of the hair follicle; it appear as little pus bumps scattered throughout the scalp that look similar to acne and can spread. The bumps can sometimes feel sore.
What it looks like: scattered pus bumps. On darker skin tones, the bumps may be a dark shade of red or light purple around the periphery.
The causes:
- Bacteria (most commonly a staph infection) or a fungal infection.
- Irritation from shaving, heavy conditioners, potent hair dyes and excessive sweating.
The treatments:
- Topical or oral antibiotics may be prescribed if your doctor determines via a culture that bacteria is causing your scalp woes.
- Anti-inflammatory medications, such as topical steroid formulations, can be effective if there isn't an infectious agent present, says Christine Ko, M.D., professor of Dermatology and Pathology at Yale School of Medicine and author of the book How to Improve Doctor-Patient Connection.
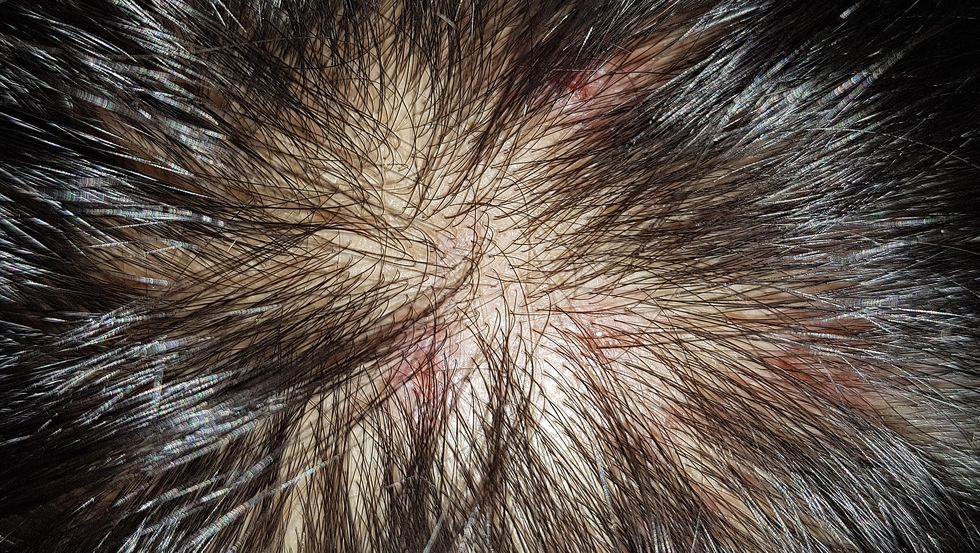
Hair loss
"Hair loss can be due to a number of different factors, including genetics, medications, inflammation, hormonal abnormalities and hair fragility," says Dr. Ko. Regardless of the cause of hair loss, it can be extremely distressing. If you notice your hair breaking or shedding, or you see bald spots on your scalp, make an appointment to get evaluated by a health care provider immediately.
What it looks like: anything from hair breaking or shedding, to bald spots on your scalp.
The causes:
- Anemia, vitamin deficiency, thyroid abnormalities, irregular hormone levels and autoimmune markers can all lead to hair loss.
- Extreme stress, such as the death of a loved one, can have an impact on your whole body including your hair.
- Major weight loss (sometimes related to a high-protein diet) can also trigger hair loss.
- Infection and illness can cause a massive shedding months after the incident — a condition called telogen effluvium. For instance, a survey conducted by Survivor Corps found that nearly 68% of 1,700 COVID-19 survivors that were interviewed reported experiencing hair loss in the wake of their coronavirus infection. "Actress Alyssa Milano even took to Twitter to describe her experienced with COVID-19-related hair loss," notes Dr. Lenzy.
- Age can also play a role: As estrogen levels decrease between childbearing age and menopause, our hair may thin out. Years of bleaching, dyeing, straightening, perming and rocking tight, slicked-back hairstyles can also catch up to us.
The treatments:
- Rogaine, a solution that thickens existing hair, and spironolactone, a pill that helps block hormones called androgens, can be helpful in cases of hormonal thinning.
- Eating a well-balanced diet is also useful when experiencing hair health woes, and talking to your doctor about whether you're deficient in iron or specific vitamins.
- Taking a break from over-processing your hair and wearing more natural styles is recommended.
- "Platelet-rich plasma (PRP) is an effective option for androgenetic alopecia (also called male and female pattern hair loss) and the residual thinning after telogen effluvium," says Dr. Lenzy. "During PRP, a patient's blood is drawn and the plasma, which is rich in various growth factors effective for stimulating hair regrowth, is isolated and injected or applied to the scalp with microneedling."
Cysts
Cysts can occur on the skin, just like they can show up on other organs. The good news: Scalp cysts are common and easy to identify. They are usually bumps the size of marbles or grapes, and you can feel them when your comb or brush runs over them. If you're unsure about a bump or you can't get a good look at your scalp, that's a smart time to consult a derm.
What it looks like: a skin-colored or pink-red smooth bump
The cause:
- For the most part, scalp cysts are mostly genetic.
The treatments:
- Leave them alone. This is definitely an easy option if the scalp cysts aren't bothering you, since they are mostly benign and shouldn't raise any concern.
- Have them drained: In some cases, however, scalp cysts can get infected or irritated, which causes pain. Incision and drainage can help calm the symptoms, but won't remove the cyst in its entirety, says Onyeka Obioha, M.D., board-certified dermatologist at Cedars Sinai in Los Angeles.
- Consider antibiotics: These can also help relieve symptoms of an inflamed or infected cyst.
- Have them surgically removed by a medical professional. Cysts contain a fluid-filled sac. "Unless the sac is removed, the cyst can recur, thus surgery is the only effective option to completely remove a cyst and make sure it doesn't recur," says Dr. Obioha. But the surgical removal is very simple and done with just a local anesthetic. While it does leave a scar, Dr. Obioha says it's often not noticeable since it's hidden by the hair.
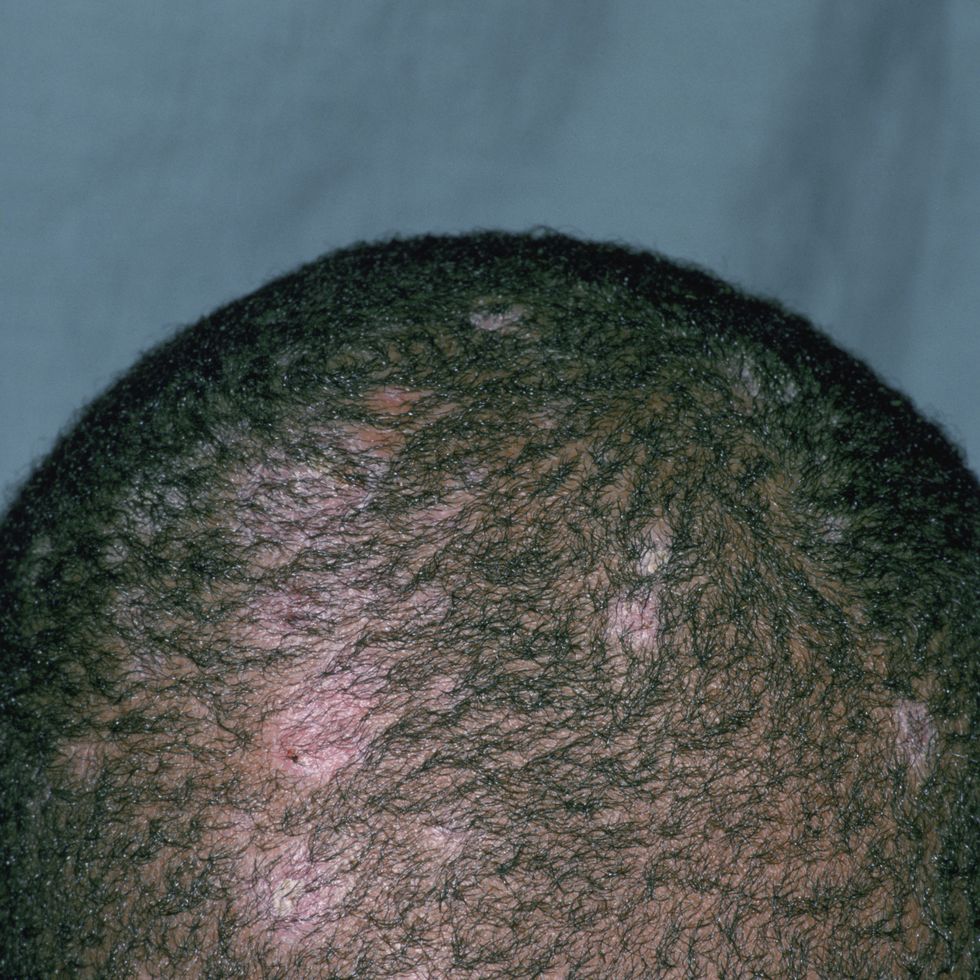
Ringworm
Also called tinea capitis, ringworm is a contagious fungal infection that usually happens in little kids, but occasionally adults get it too. Despite the name, no worm is involved: The condition got its name from its circular shape. The rash is usually painful and scaly, sometimes even causing enlarged lymph nodes. It also can lead to bald spots, broken hairs and black dots on the skin.
What it looks like: scaly rash and bald spots
The cause:
- According to the Mayo Clinic, there are a few ways of contracting the fungus directly: human to human, animal to human (cats are a common source) and object (like clothing, towels, bedding, combs and brushes) to human. "Ringworm can also be transferred by indirect contact through a swimming pool or hot tub," says Dr. Obioha.
The treatment:
- Antifungal medication taken daily for 4 to 6 weeks usually does the job of eliminating ringworm. "Ringworm is no longer contagious 48 hours after starting treatment," says Dr. Obioha. Until then, "you want to avoid contact with others, as tinea capitis can spread through contact with other areas of the body and other people," she adds.
Allergic Contact Dermatitis (ACD)
This rash is a reaction to the scalp coming into direct contact with an allergen that results in a response from the immune system—sometimes days after the contact, so it can be difficult to determine what the body is reacting to. "ACD can be painful, itchy and even oozing in some cases," says Dr. Obioha. The symptoms of a severe case can often be mistaken for infection.
What it looks like: itchy redness. On darker skin tones, it may look pink, grayish, or purple
The causes:
- Paraphenylenediamine (PPD) is a chemical that is widely used as a permanent hair dye and it can wreak havoc on the skin and is one of the most common causes of scalp allergic contact dermatitis.
- The chemicals/fragrances in shampoos and conditioners are also a common cause of ACD.
- "Other relevant possible allergens include propylene glycol, Cocamidopropyl betaine, methylisothiazolinone (MI) or a combined formulation of methylchloroisothiazolinone and MI," says Dr. Obioha.
The treatments:
- Identifying the trigger and eliminating it. As stated, that can be difficult to determine; sometimes a patch test is needed to figure out what the body is allergic to.
- Topical steroid gel, foam, cream or ointment: Two to three weeks of treatment should help decrease inflammation and clear up your skin. "Systemic steroids may be prescribed in severe cases," adds Dr. Obioha.
*With additional reporting by Kaitlyn Phoenix, Marisa Cohen and Lisa Bain
With more than a decade of experience, board-certified dermatologist Caroline Chang, M.D., is nationally recognized as a top doctor in both medical and cosmetic dermatology. She is also the founder of Rhode Island Dermatology Institute, the state’s first direct care dermatology practice with the goal of providing high-quality, customized care.