Human Papilloma Virus and Cervical Cancer
Human Papilloma Virus and Cervical Cancer
Since January is Cervical Health Awareness Month, I’m going to write for the first time about a tough topic I’ve been discussing with women for over 30 years. The topic is the human papillomavirus, aka HPV.
The first HPV test was FDA approved in 1988. I started my OB/GYN residency program in 1990. I remember using the little cotton swab at the same time that we did the Pap smear to do this new screening. This was when we had to actually do a “smear” onto a glass slide. The Pap technology quickly advanced to become liquid cytology, which could check the cervical cells and the HPV status in one sample to the lab (no fumbling around with a glass slide required).
HPV testing is important because out of the more than 150 HPV genotypes, we can now test for 14 genotypes associated with cervical cancer. Of these types, they are divided into high, middle and low risk for causing cervical cancer. (The low risk types are associated with condyloma, or genital warts, and are not my topic today.)
How common is cervical cancer and how quickly does it grow?
In the United States, there are just over 14,000 new cases of cervical cancer every year. Cervical cancer causes just over 4,000 deaths among women in the US every year.
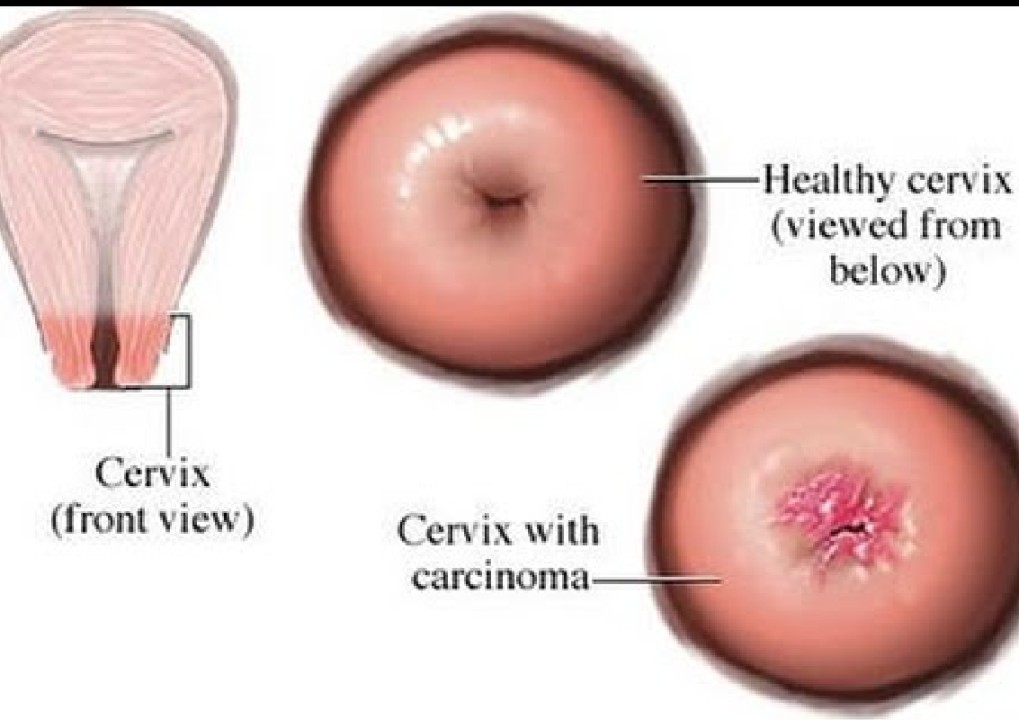
In several large long-term studies, women with high risk types of HPV had up to a 48% risk of developing cervical carcinoma in situ (CIS), the level of abnormal cells right before cervical cancer. I want to emphasize that it took at least five years for the abnormal cervical cells to get to this pre-cancer level. The low risk types of HPV on the other hand, when watched for at least five years, resulted in CIS less than 10% of the time.
What does this mean?
These findings show that in most healthy women, the body will heal abnormal cervical cells. The biggest advantage of HPV testing is that when the test is negative or shows low risk HPV types, she can be followed over time with Pap tests, without having to go through the pain and worry of cervical biopsies. In young women, especially teenagers, over-treatment of abnormal cervical cells can cause scarring on the cervix. This can lead to problems later in life with pregnancy or childbirth.
In areas of the world with limited access to healthcare, a home test for HPV can be done as a screening test. A woman only needs to be seen by a healthcare provider for a Pap test if she has any of the middle or high risk types of HPV.
How common is HPV?
The estimates I have come across say that 80% of women will be infected with HPV over their lifetime. I think the statistic is closer to 100% of women who have ever had any kind of sexual contact.
HPV can hang around in the cervical and vaginal environment for many years, even decades. For a woman who tests positive for HPV, it can be very difficult to know when she was exposed.
At this time, all the organizations that have developed Pap and HPV testing algorithms recommend stopping screening at age 65. I disagree with this because we know that sexually transmitted infections, including HPV, are rising among people over 65, as they are living in community settings and having new (and sometimes multiple) sexual partners. Screening for cervical cancer with both Pap and HPV testing should, as with other screening tests, be used not only by protocol but also based on the needs of the individual.
Do men get HPV?
Absolutely. Men get HPV the same way women do, mainly through sexual exposure. The main reason men do not get tested routinely for HPV is that their genital skin is exposed to air and can stay dry, therefore they very rarely develop problems.
HPV in men can cause cancer of the penis. Again, because they do not have the warm moist environment of the vagina, penile cancer is diagnosed in fewer than one in 100,000 men in North America and Europe each year. Any condition that creates a warm moist environment can raise a man’s risk for HPV causing cancer of the penis. This includes not being circumcised or phimosis, a condition where the foreskin is difficult to retract. In both of these situations, HPV can thrive and cause abnormal cells to develop.
Can you get rid of HPV?
This is a tough question because HPV is a virus, and our bodies constantly are exposed to and carry viruses. The biggest healer of HPV is good general health and time. By general health, I include not smoking and getting good basic nutrition.
Just as we don’t have a goal of being 100% free of the common cold virus in our lungs, the goal is not to get completely rid of HPV. Instead, the goal is to do everything else that we can to stay healthy and keep symptoms – and abnormal cell changes – at bay.
In my line of work, I cannot say “always” or “never.” BUT…
Cervical cancer is one of the most preventable female cancers.
At least half of the women who develop cervical cancer have never had a Pap test. If you or someone you know has HPV, the situation will “never” lead to cervical cancer as long as you get good follow up care.
Talk with your primary care doctor or your gynecologist to get Pap and HPV screening tests according to your personal situation, not only according to a protocol.



