Pancreas (Human Anatomy): Image, Function, Conditions, Tests, Treatments
Last Updated: Feb 25, 2023
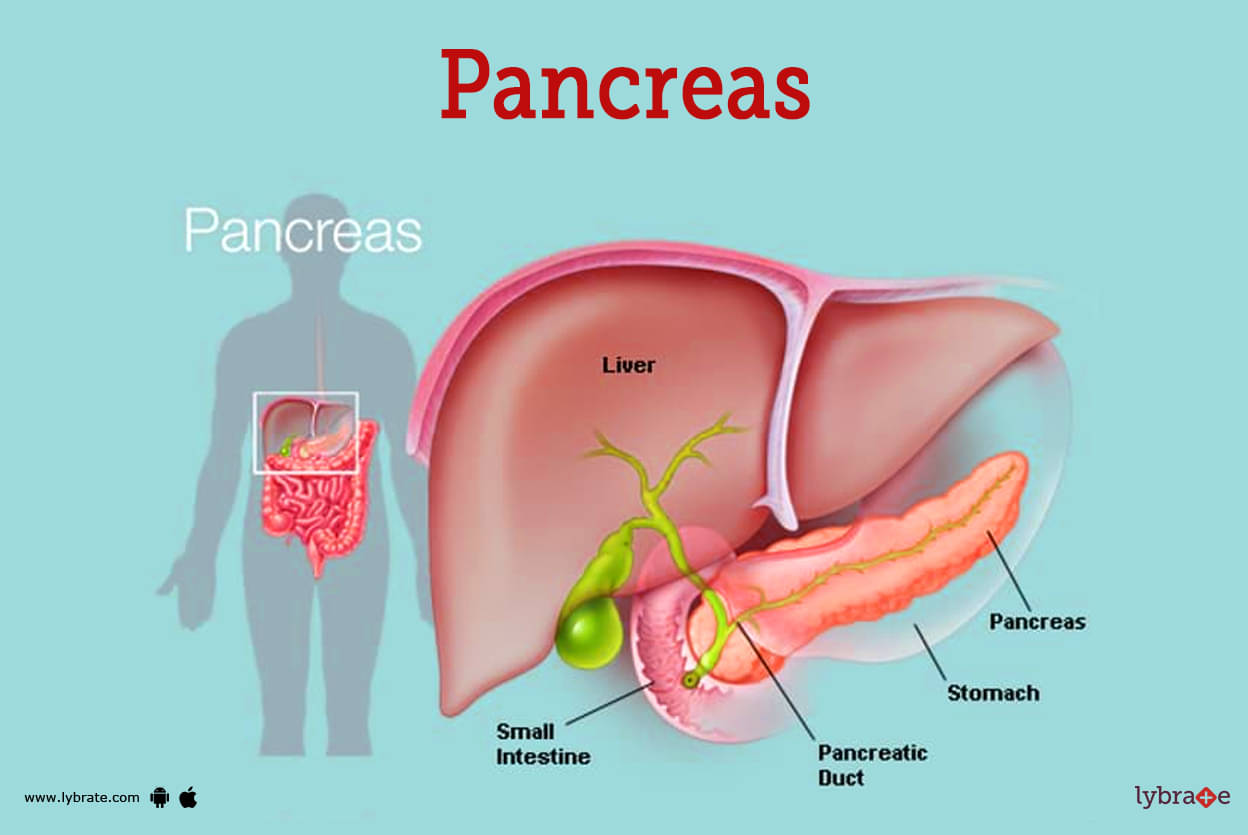
Pancreas Image
The pancreas is an organ as well as a gland. Glands are organs in the body that generate and release chemicals. The pancreas has two primary functions: exocrine and endocrine. Exocrine function: produces chemicals (enzymes) that aid in digesting. Endocrine function: Secretes hormones that regulate the quantity of sugar in the circulation.
The pancreas has the shape of a J' or a retort because it is positioned at an angle. The retort's bowl stands in for the animal's head, while the stem of the retort depicts the animal's neck, body, and tail.
In addition to being situated in the epigastric and left hypochondriac regions, the pancreas occupies a position on the posterior abdominal wall that is roughly horizontal. From the concavity of the duodenum, where it begins, it makes an oblique journey across the posterior abdominal wall until it reaches the hilum of the spleen, which is located on the opposite side of the level of the T12-13 vertebrae.
Functions of Pancreas
The pancreas has two main functions:
- Exocrine function: The pancreas produces enzymes that help to digest food in the small intestine. These enzymes include amylase, which breaks down carbohydrates; lipase, which breaks down fats; and trypsin and chymotrypsin, which breaks down proteins. The process of pancreatic secretion involves chemical work and is linked to an increase in the amount of oxygen that is consumed. The pancreatic duct cells contain carbonic anhydrase, which allows them to produce the hydrogen carbonate that is then expelled into the duct lumen.
- Endocrine function: The pancreas also produces hormones, including insulin and glucagon, which help to regulate blood sugar levels. Insulin promotes the uptake of glucose into cells, while glucagon promotes the release of glucose from the liver.
Overall the pancreas plays a vital role in maintaining the body's metabolism and energy balance.
Pancreas Conditions
- Diabetes, type 1: Diabetes type 1 is a condition that is considered to be chronic. Insulin-producing cells in the pancreas are targeted for destruction by the immune system of the body. As a result, either none or a very small amount of insulin is produced.Insulin injections are required for the rest of one's life in order to maintain blood sugar control.It is also known as juvenile diabetes or insulin-dependent diabetes
- Diabetes, type 2: One form of diabetes mellitus is known as type 2 diabetes, which was formerly referred to as adult-onset diabetes. The body develops a resistance to insulin, which leads to an increase in blood sugar levels in people with diabetes type 2. Eventually, the pancreas will lose its capacity to produce and secrete insulin appropriately, which will necessitate the use of insulin that is manufactured in a lab.
- Cystic fibrosis: Cystic fibrosis is a genetic disorder that can affect multiple organs and body systems, the most common of which are the lungs and the pancreas. Digestive problems and diabetes often result.
- Pancreatic cancer: There are many different kinds of cells that can be found in the pancreas, and each of these cell kinds has the potential to develop into a different kind of tumour if it becomes malignant. The cells that line the pancreatic duct are where the most common form of pancreatic cancer begins to develop. Because there are typically very few or no early symptoms, pancreatic cancer is typically found in an advanced stage by the time it is identified. This is because early detection is difficult.
- Pancreatitis: When exposed to the pancreas' own digestive chemicals, the organ experiences irritation and can sustain damage. As a direct result of this, the tissue of the pancreas may swell and eventually pass away. There are cases in which the root cause of pancreatitis cannot be pinpointed, despite the fact that alcohol consumption and gallstone formation are both potential contributors.
- Pancreatic pseudocyst: After an episode of pancreatitis, a cavity called a pseudocyst may develop in the pancreas. This cavity is filled with fluid. Pseudocysts may resolve on their own, or a surgeon may need to drain them surgically in order for them to disappear.
- Islet cell tumor: The proliferation of hormone-producing cells in the pancreas in an abnormal manner, which may or may not result in the development of a malignant tumour. These tumours produce an abnormally high level of hormones, which the rest of the body then responds to by releasing them into the bloodstream. Gastrinomas, glucagonomas, and insulinomas are all examples of islet cell tumours; however, this list is not exhaustive.
- Enlarged pancreas: An enlarged pancreas is a rare condition to experience in people. It is possible that this is just a harmless anatomic abnormality, but it is also possible that it is a sign of autoimmune pancreatitis. Either way, it is important to get it checked out.
- Annular pancreas: A developmental abnormality known as annular pancreas is characterised by the presence of a ring of pancreatic tissue that surrounds the second portion of the duodenum.
- Accessory pancreatic tissue: It is possible to have accessory pancreatic tissue in the following locations: (a) the wall of the stomach; (b) the duodenum (this is the most common location); (e) the small intestine; (d) Meckel's diverticulum; (e) the great omentum; and (f) the hilum of the spleen. It manifests itself as lobulated nodules that are yellowish in colour and typically range in diameter from one to six millimetres. Roughly one-third of these nodules contain islets of Langerhans.
- Carcinoma of the head of pancreas: The cancer of the head of the pancreas occurs usually. It causes persistent obstructive jaundice as a result of the compression of the bile duct. Due to the close proximity of these structures to the head of the pancreas, it may exert pressure on the portal vein or it may involve the stomach.
- Acute pancreatitis: The acute inflammation of the pancreas is referred to as acute pancreatitis. It can be brought on by an obstruction of the pancreatic duct, the consumption of alcohol, viral infections (such as mumps), or trauma. In the clinical setting, symptoms include severe pain in the epigastric region that spreads to the back, fever, nausea, and vomiting. There was a significant increase in the amount of amylase in the serum.
- Chronic Pancreatitis: It is a disorder that gets progressively worse and is associated with the pancreas getting destroyed. This condition is more prevalent in males and typically manifests itself in individuals between the ages of 30 and 40. Pain in the upper abdominal region and diarrhoea are the symptoms that are most frequently experienced.
Pancreas Tests
- Physical examination: A doctor may examine for lumps or abdominal discomfort by pushing on the middle of the patient's stomach. Pain in the pancreas can frequently be felt in the back. They can also search for additional symptoms that may indicate a problem affecting the pancreas.Abdominal ultrasound: A whole abdominal ultrasound can cause obstruction of the secretion of pancreas. It also can show an abscess or a pancreatic pseudocyst.
- Abdominal CT: A diagnostic imaging examination known as a computed tomography (CT) scan of the abdomen and pelvis can be performed. During an abdominal CT scan, a specialised X-ray machine is used to capture images of the patient's organs, including the intestines, pancreas, and adrenal glands.The consequences of pancreatic illness, such as fluid surrounding the pancreas, an enclosed infection (abscess), or a collection of tissue, fluid, and pancreatic enzymes, can be identified using a CT scan (pancreatic pseudocyst).
- MRI: It stands for magnetic resonance imaging, for which high resolution imaging is done by using a super magnetic conductor and a central processing unit, which involves resizing and impartial diagnosis of disorders of bones, heart, spleen, kidney and other vital organs.ERCP (Endoscopic Retrograde Cholangiopancreatography): A long, flexible tube with a camera and equipment on the end is used in ERCP (Endoscopic Retrograde Cholangiopancreatography), a procedure that allows doctors to diagnose and even treat some pancreatic conditions.
- Pancreas biopsy: Tests for cancer and other disorders sometimes require removing a small piece of pancreatic tissue from the body, which can be done with a needle inserted under the skin or through surgery.
- Endoscopic ultrasound: The belly is probed with an ultrasonic probe, and harmless sound waves bounce off internal organs to generate images. When an invasive test like ERCP may aggravate the patient's condition, an endoscopic ultrasound may be a lifesaver in finding gallstones and diagnosing severe pancreatitis. This ultrasonic approach can also be utilised to get a sample of pancreatic tissue for analysis or a biopsy.
- Serum Amylase and lipase: When blood tests show excessively high levels of the pancreatic enzymes in question, pancreatitis may be considered.
- Sweat chloride test: We test the chloride concentration in sweat by applying a painless electric current to the skin. People with cystic fibrosis often sweat excessively, and this chlorine can be detected in their breath.
- Genetic testing: Many different types of gene mutations have been linked to the onset of cystic fibrosis. Through genetic testing, it is possible to ascertain not only whether or not a child will be affected by cystic fibrosis but also whether or not an adult is a carrier for the disease.
- Magnetic resonance cholangiopancreatography (MRCP): This kind of magnetic resonance imaging (MRI) can be used to look at the bile ducts and the pancreatic duct.
- Secretin stimulation test: The hormone secretin stimulates the pancreas to secrete a digestive fluid that reduces stomach acid. The secretin stimulation test measures the level of secretin sensitivity in the pancreas. Pancreatic diseases patients may undergo this test to gauge pancreatic function (for example, cystic fibrosis or pancreatic cancer).
- Fine needle aspiration cytology: A syringe is furnished with suction, and a needle with a very small gauge is introduced into the pancreatic mass. The needle is then moved back and forth while it is still inside the pancreatic mass.
- Faecal elastase test: Another method of gauging pancreatic health is the faecal elastase test. As an enzyme produced by the pancreas, elastase is the target of this test. Elastase is a protein digesting enzyme. The presence of elastase in a patient's faeces is evaluated in this test.
Pancreas Treatments
- Insulin: Injecting insulin under the skin causes body tissues to absorb glucose, lowering blood sugar. Insulin can be created in a lab or purified from animal sources.
- Pseudocyst drainage: A pseudocyst can be drained by inserting a tube or needle through the skin into the pseudocyst. Alternately, a small tube or stent is placed between either the pseudocyst and the stomach or the small intestine, draining the cyst.
- Pseudocyst surgery: Sometimes, surgery is necessary to remove a pseudocyst. Either laparoscopy (multiple small incisions) or laparotomy (one larger incision) may be needed.
- Pancreatic cancer resection (Whipple procedure): The standard surgery to remove pancreatic cancer. In a Whipple procedure, a surgeon removes the head of the pancreas, the gallbladder, and the first section of the small intestine (the duodenum). Occasionally, a small part of the stomach is also removed.
- Pancreas transplantation: An organ donor’s pancreas is transplanted into someone with diabetes or cystic fibrosis. In some patients, a pancreas transplant cures diabetes.
- Islet cell transplantation: Insulin-producing cells are harvested from an organ donor’s pancreas and transplanted into someone with type 1 diabetes. The still-experimental procedure can potentially cure type 1 diabetes.
- Pancreatic stenting/pancreatic endotherapy: A stent may be placed in a narrow or blocked pancreatic duct to widen it or to drain extra fluid. It is also used to relieve pain.
- Necrosectomy: The endoscopic draining and debridement of pancreatic necrosis is referred to as endoscopic pancreatic necrosectomy. The ultimate objective of necrosectomy is to eliminate all regions of infection and necrosis. The necrotic pancreatic tissues and debris are carefully removed using forceps.
- Pancreaticoduodenectomy: The most common operation for treating pancreatic cancer is pancreaticoduodenectomy. Because organs in the proximal gastrointestinal system share a blood supply, surgical removal of the pancreatic head entails removal of the duodenum, proximal jejunum, gallbladder, and, in certain cases, a portion of pancreas.
Pancreas Medicines
Rapid insulin therapy Treatment of diabetes mellitus with rapid-acting insulin has been shown to be effective. Lispro and Aspart are two examples with an hourly peak action rate.
- Short insulin therapy: Insulin treatment refers to the administration of insulin that has a bio availability of an operating time of two to four hours at most and is sold under the trade name of normal insulin.
- Long insulin: Examples of this kind of treatment are the insulins Degludec, Detemir, and Glargine, each of which has a bio availability or working duration of 24 hours.
- Biguanides: Biguanides, such as metformin, are used to treat diabetes mellitus because they enhance gluconeogenesis while simultaneously lowering peripheral glucose absorption. These hypoglycemic medications are necessary for the continued maintenance of glucose metabolism.
- Sulfonylurea: effective in treating diabetes mellitus because they work by stimulating pancreatic cells to create insulin Glipizide, Glyburide, and Glimepiride are just a few of the medications that fall under this category.
- Thiazolidinedione: beneficial in lowering one's insulin resistance, which can act as a therapy for diabetes either directly or indirectly. Pioglitazone Rosiglitazone
- SGLT-2, Inhibitor: Canagliflozin, Dapagliflozin, and Empagliflozin are a few examples of the types of medications that have been shown to be effective at inhibiting SGLT 2 channels and so assisting in the maintenance of normal glucose metabolism.
Frequently Asked Questions (FAQs)
What are the warning signs of the pancreas?
Can you live without a pancreas?
What happens when your pancreas has problems?
What causes the pancreas to have problems?
How do you check your pancreas?
Where is pancreas pain usually felt?
What puts stress on the pancreas?
Can your pancreas heal itself?
How serious is pancreatic surgery?
How does pancreatitis cause death?
Table of content
Find Gastroenterologist near me
Ask a free question
Get FREE multiple opinions from Doctors