Erythema Nodosum in Children: A Narrative Review and a Practical Approach
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Epidemiology
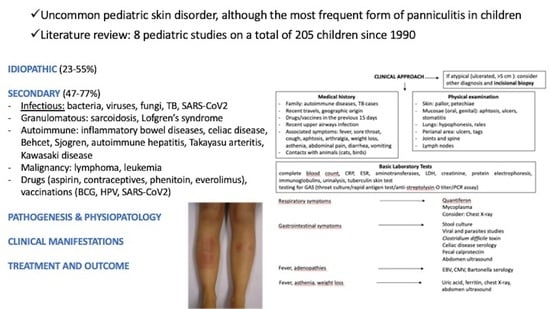
3.2. Etiology
3.2.1. Infectious Diseases
3.2.2. Systemic Diseases
3.2.3. Malignancy
3.2.4. Others
3.3. Pathophysiology and Histopathology
3.4. Clinical Presentation
3.5. Assessment and Diagnosis
3.6. Prognosis
3.7. Treatment
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blake, T.; Manahan, M.; Rodins, K. Erythema nodosum—A review of an uncommon panniculitis. Dermatol. Online J. 2014, 20, 22376. [Google Scholar] [CrossRef]
- Leung, A.K.C.; Leong, K.F.; Lam, J.M. Erythema nodosum. World J. Pediatr. 2018, 14, 548–554. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, R.A.; Nervi, S.J. Erythema nodosum: A sign of systemic disease. Am. Fam. Physician 2007, 75, 695–700. [Google Scholar] [PubMed]
- Porges, T.; Shafat, T.; Sagy, I.; Zeller, L.; Bartal, C.; Khutarniuk, T.; Jotkowitz, A.; Barski, L. Clinical, epidemiological, and etiological changes in erythema nodosum. Isr. Med. Assoc. J. 2018, 20, 770–772. [Google Scholar]
- Labbé, L.; Perel, Y.; Maleville, J.; Taïeb, A. Erythema nodosum in children: A study of 27 patients. Pediatr. Dermatol. 1996, 13, 447–450. [Google Scholar] [CrossRef] [PubMed]
- Mert, A.; Kumbasar, H.; Ozaras, R.; Erten, S.; Tasli, L.; Tabak, F.; Ozturk, R. Erythema nodosum: An evaluation of 100 cases. Clin. Exp. Rheumatol. 2007, 25, 563–570. [Google Scholar] [PubMed]
- Kakourou, T.; Drosatou, P.; Psychou, F.; Aroni, K.; Nicolaidou, P. Erythema nodosum in children: A prospective study. J. Am. Acad. Dermatol. 2001, 44, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Elkayam, O.; Caspi, D.; Segal, R.; Brautbar, C.; Ben-Chetrit, E.; Yaron, M. Familial erythema nodosum. Arthritis Rheum. 1991, 34, 1177–1179. [Google Scholar] [CrossRef] [PubMed]
- García-Porrúa, C.; González-Gay, M.A.; Vázquez-Caruncho, M.; López-Lazaro, L.; Lueiro, M.; Fernández, M.L.; Alvarez-Ferreira, J.; Pujol, R.M. Erythema nodosum: Etiologic and predictive factors in a defined population. Arthritis Rheum. 2000, 43, 584–592. [Google Scholar] [CrossRef]
- Hassink, R.I.; Pasquinelli-Egli, C.E.; Jacomella, V.; Laux-End, R.; Bianchetti, M.G. Conditions currently associated with erythema nodosum in Swiss children. Eur. J. Pediatr. 1997, 156, 851–853. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aydın-Teke, T.; Tanır, G.; Bayhan, G.I.; Metin, O.; Oz, N. Erythema nodosum in children: Evaluation of 39 patients. Turk. J. Pediatr. 2014, 56, 144–149. [Google Scholar] [PubMed]
- Picco, P.; Gattorno, M.; Vignola, S.; Barabino, A.; Marazzi, M.G.; Bondi, E.; Pistoia, V.; Buoncompagni, A. Clinical and biological characteristics of immunopathological disease-related erythema nodosum in children. Scand. J. Rheumatol. 1999, 28, 27–32. [Google Scholar] [PubMed]
- Cengiz, A.B.; Kara, A.; Kanra, G.; Seçmeer, G.; Ceyhan, M. Erythema nodosum in childhood: Evaluation of ten patients. Turk. J. Pediatr. 2006, 48, 38–42. [Google Scholar] [PubMed]
- Garty, B.Z.; Poznanski, O. Erythema nodosum in Israeli children. Isr. Med. Assoc. J. 2000, 2, 145–146. [Google Scholar] [PubMed]
- Litwin, L.; Machura, E. The etiology and clinical manifestation of erythema nodosum in hospitalized children—Analysis of 12 cases. Preliminary report. Dev. Period Med. 2014, 18, 506–512. [Google Scholar] [PubMed]
- Pérez-Garza, D.M.; Chavez-Alvarez, S.; Ocampo-Candiani, J.; Gomez-Flores, M. Erythema nodosum: A practical approach and diagnostic algorithm. Am. J. Clin. Dermatol. 2021, 22, 367–378. [Google Scholar] [CrossRef] [PubMed]
- Greco, F.; Catania, R.; Pira, A.L.; Saporito, M.; Scalora, L.; Aguglia, M.G.; Smilari, P.; Sorge, G. Erythema Nodosum and Mycoplasma pneumoniae Infections in Childhood: Further Observations in Two Patients and a Literature Review. J. Clin. Med. Res. 2015, 7, 274–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimizu, M.; Hamaguchi, Y.; Matsushita, T.; Sakakibara, Y.; Yachie, A. Sequentially appearing erythema nodosum, erythema multiforme and Henoch-Schönlein purpura in a patient with Mycoplasma pneumoniae infection: A case report. J. Med. Case Rep. 2012, 6, 398. [Google Scholar] [CrossRef] [Green Version]
- Wallis, P.; Starr, M.; Phillips, R.J. An uncommon cause of erythema nodosum. J. Paediatr. Child Health 2016, 52, 961–963. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, C.C.; Neves, F.L.; Cardoso, P.N. Tuberculosis presenting as erythema nodosum in childhood. J. Paediatr. Child Health 2022. [Google Scholar] [CrossRef]
- Kritsotakis, E. Erythema nodosum as sign of primary tuberculosis. Oxf. Med. Case Rep. 2017, 2017, omx041. [Google Scholar] [CrossRef] [Green Version]
- Ariza-Prota, M.; Pando-Sandoval, A.; García-Clemente, M.; Casan, P. Poncet’s disease mimicking rheumatoid arthritis in a patient with suspected Crohn’s disease. Clin. Case Rep. 2016, 4, 72–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mantadakis, E.; Arvanitidou, V.; Tsalkidis, A.; Thomaidis, S.; Chatzimichael, A. Erythema nodosum associated with Salmonella enteritidis. Hippokratia 2010, 14, 51–53. [Google Scholar] [PubMed]
- Diolombi, M.; Seneviratne, M.; Norton, R. Case report: Erythema nodosum and melioidosis: An unreported association. Am. J. Trop. Med. Hyg. 2020, 103, 1841–1843. [Google Scholar] [CrossRef]
- Suter, P.; Mooser, B.; Pham Huu Thien, H.P. Erythema nodosum as a cutaneous manifestation of COVID-19 infection. BMJ Case Rep. 2020, 13, e236613. [Google Scholar] [CrossRef]
- Parker, E.R.; Fitzpatrick, A. A case report of COVID-19-associated erythema nodosum: A classic presentation with a new trigger. Fam. Pract. 2022. [Google Scholar] [CrossRef] [PubMed]
- Body, B.A. Cutaneous manifestations of systemic mycoses. Dermatol. Clin. 1996, 14, 125–135. [Google Scholar] [CrossRef]
- Zaraa, I.; Trojjet, S.; El Guellali, N.; El Euch, D.; Chelly, I.; Mokni, M.; Zitouna, M.; Osman, A.B. Childhood erythema nodosum associated with kerion celsi: A case report and review of literature. Pediatr. Dermatol. 2012, 29, 479–482. [Google Scholar] [CrossRef]
- Yanardağ, H.; Pamuk, O.N.; Karayel, T. Cutaneous involvement in sarcoidosis: Analysis of the features in 170 patients. Respir. Med. 2003, 97, 978–982. [Google Scholar] [CrossRef] [Green Version]
- Fauroux, B.; Clément, A. Paediatric sarcoidosis. Paediatr. Respir. Rev. 2005, 6, 128–133. [Google Scholar] [CrossRef]
- Brown, F.; Modi, P.; Tanner, L.S. Lofgren Syndrome; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Komishke, B.; Foulds, J.L.; McMillan, T.; Avdimiretz, N. Bilateral leg swelling as the presenting symptom of Löfgren syndrome in a paediatric patient: A rare presentation of a rare paediatric disease. BMJ Case Rep. 2021, 14, e239434. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, M.; Turner, D.; Avitzur, Y. Erythema nodosum as a presentation of inflammatory bowel disease. Can. Med. Assoc. J. 2005, 173, 145–146. [Google Scholar] [CrossRef] [PubMed]
- Timani, S.; Mutasim, D.F. Skin manifestations of inflammatory bowel disease. Clin Dermatol 2008, 26, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Vavricka, S.R.; Schoepfer, A.; Scharl, M.; Lakatos, P.L.; Navarini, A.; Rogler, G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm. Bowel Dis. 2015, 21, 1982–1992. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antonelli, E.; Bassotti, G.; Tramontana, M.; Hansel, K.; Stingeni, L.; Ardizzone, S.; Genovese, G.; Marzano, A.V.; Maconi, G. Dermatological manifestations in inflammatory bowel diseases. J. Clin. Med. 2021, 10, 364. [Google Scholar] [CrossRef] [PubMed]
- Dotson, J.L.; Hyams, J.S.; Markowitz, J.; LeLeiko, N.S.; Mack, D.R.; Evans, J.S.; Pfefferkorn, M.D.; Griffiths, A.M.; Otley, A.R.; Bousvaros, A.; et al. Extraintestinal manifestations of pediatric inflammatory bowel disease and their relation to disease type and severity. J. Pediatr. Gastroenterol. Nutr. 2010, 51, 140–145. [Google Scholar] [CrossRef]
- Misago, N.; Tada, Y.; Koarada, S.; Narisawa, Y. Erythema nodosum-like lesions in Behçet’s disease: A clinicopathological study of 26 cases. Acta Derm. Venereol. 2012, 92, 681–686. [Google Scholar] [CrossRef] [Green Version]
- Bartyik, K.; Várkonyi, A.; Kirschner, A.; Endreffy, E.; Túri, S.; Karg, E. Erythema nodosum in association with celiac disease. Pediatr. Dermatol. 2004, 21, 227–230. [Google Scholar] [CrossRef]
- Fretzayas, A.; Moustaki, M.; Liapi, O.; Nicolaidou, P. Erythema nodosum in a child with celiac disease. Case Rep. Pediatr. 2011, 2011, 935153. [Google Scholar] [CrossRef]
- He, S.; Zhen, X.; Hu, Y. Juvenile primary Sjogren’s syndrome with cutaneous involvement. Clin. Rheumatol. 2021, 40, 3687–3694. [Google Scholar] [CrossRef]
- Meier, K.; Schloegl, A.; Poddubnyy, D.; Ghoreschi, K. Skin manifestations in spondyloarthritis. Ther. Adv. Musculoskelet Dis. 2020, 12, 1759720X20975915. [Google Scholar] [CrossRef] [PubMed]
- Gallizzi, R.; Pidone, C.; Cantarini, L.; Finetti, M.; Cattalini, M.; Filocamo, G.; Insalaco, A.; Rigante, D.; Consolini, R.; Maggio, M.C.; et al. A national cohort study on pediatric Behçet’s disease: Cross-sectional data from an Italian registry. Pediatr. Rheumatol. Online J. 2017, 15, 84. [Google Scholar] [CrossRef] [Green Version]
- Koné-Paut, I.; Shahram, F.; Darce-Bello, M.; Cantarini, L.; Cimaz, R.; Gattorno, M.; Anton, J.; Hofer, M.; Chkirate, B.; Bouayed, K.; et al. PEDBD group Consensus classification criteria for paediatric Behçet’s disease from a prospective observational cohort: PEDBD. Ann. Rheum. Dis. 2016, 75, 958–964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abenavoli, L.; Dastoli, S.; Bennardo, L.; Boccuto, L.; Passante, M.; Silvestri, M.; Proietti, I.; Potenza, C.; Luzza, F.; Nisticò, S.P. The skin in celiac disease patients: The other side of the coin. Medicina 2019, 55, 578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kavehmanesh, Z.; Beiraghdar, F.; Saburi, A.; Hajihashemi, A.; Amirsalari, S.; Movahed, M. Pediatric autoimmune hepatitis in a patient who presented with erythema nodosum: A case report. Hepat. Mon. 2012, 12, 42–45. [Google Scholar] [CrossRef]
- Loetscher, J.; Fistarol, S.; Walker, U.A. Pyoderma gangrenosum and erythema nodosum revealing takayasu’s arteritis. Case Rep. Dermatol. 2016, 8, 354–357. [Google Scholar] [CrossRef] [PubMed]
- Okada, S.; Ishikawa, Y.; Shimomura, M.; Sunagawa, S.; Hirano, R.; Fukunaga, S.; Miyake, A.; Okada, Y.; Maki, T. Erythema Nodosum Masking Kawasaki Disease with an Initial Manifestation of Skin Lesions. Yonsei Med. J. 2019, 60, 312–314. [Google Scholar] [CrossRef] [PubMed]
- Moreira, A.; Torres, B.; Peruzzo, J.; Mota, A.; Eyerich, K.; Ring, J. Skin symptoms as diagnostic clue for autoinflammatory diseases. An. Bras. Dermatol. 2017, 92, 72–80. [Google Scholar] [CrossRef] [Green Version]
- Bjornstad, E.C.; James, K.; Culton, D.; Williams, C.; Wardrop, R.M. Erythema nodosum and fevers. Clin. Pediatr. 2015, 54, 1297–1298. [Google Scholar] [CrossRef]
- Chan, L.; Campbell, D.E.; Ming, A.G. Erythema nodosum in an adolescent patient with cryopyrin-associated periodic syndrome. Clin. Case Rep. 2018, 6, 1241–1245. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.R. Combined reduced-antigen content tetanus, diphtheria, and acellular pertussis (tdap) vaccine-related erythema nodosum: Case report and review of vaccine-associated erythema nodosum. Dermatol. Ther. 2013, 3, 191–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonci, A.; Di Lernia, V.; Merli, F.; Lo Scocco, G. Erythema nodosum and Hodgkin’s disease. Clin. Exp. Dermatol. 2001, 26, 408–411. [Google Scholar] [CrossRef] [PubMed]
- La Spina, M.; Russo, G. Presentation of childhood acute myeloid leukemia with erythema nodosum. J. Clin. Oncol. 2007, 25, 4011–4012. [Google Scholar] [CrossRef]
- Xu, X.; Liang, G.; Duan, M.; Zhang, L. Acute myeloid leukemia presenting as erythema nodosum: A case report. Medicine 2017, 96, e8666. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, R.; Clowers-Webb, H.; Davis, M.D.P. Erythema nodosum: A presenting sign of acute myelogenous leukemia. Cutis 2005, 76, 114–116. [Google Scholar] [PubMed]
- Lin, J.T.; Chen, P.M.; Huang, D.F.; Kwang, W.K.; Lo, K.; Wang, W.S. Erythema nodosum associated with carcinoid tumour. Clin. Exp. Dermatol. 2004, 29, 426–427. [Google Scholar] [CrossRef] [PubMed]
- Perez, N.B.; Bernad, B.; Narváez, J.; Valverde, J. Erythema nodosum and lung cancer. Jt. Bone Spine 2006, 73, 336–337. [Google Scholar] [CrossRef] [PubMed]
- Polcari, I.C.; Stein, S.L. Panniculitis in childhood. Dermatol. Ther. 2010, 23, 356–367. [Google Scholar] [CrossRef] [PubMed]
- Ricci, R.M.; Deering, K.C. Erythema nodosum caused by omeprazole. Cutis 1996, 57, 434. [Google Scholar] [PubMed]
- Galligan, E.R.; Fix, L.; Levin, L.E.; Imundo, L.; Yamashiro, D.J.; Garzon, M.C. Erythema nodosum arising during everolimus therapy for tuberous sclerosis complex. Pediatr. Dermatol. 2018, 35, e235–e236. [Google Scholar] [CrossRef]
- Aly, M.H.; Alshehri, A.A.; Mohammed, A.; Almalki, A.M.; Ahmed, W.A.; Almuflihi, A.M.; Alwafi, A.A. First case of erythema nodosum associated with pfizer vaccine. Cureus 2021, 13, e19529. [Google Scholar] [CrossRef] [PubMed]
- Teymour, S.; Ahram, A.; Blackwell, T.; Bhate, C.; Cohen, P.J.; Whitworth, J.M. Erythema nodosum after Moderna mRNA-1273 COVID-19 vaccine. Dermatol. Ther. 2022, e15302. [Google Scholar] [CrossRef] [PubMed]
- Cameli, N.; Silvestri, M.; Mariano, M.; Bennardo, L.; Nisticò, S.P.; Cristaudo, A. Erythema nodosum following the first dose of ChAdOx1-S nCoV-19 vaccine. J. Eur. Acad. Dermatol. Venereol. 2022, 36, e161–e162. [Google Scholar] [CrossRef]
- Requena, L.; Yus, E.S. Panniculitis. Part I. Mostly septal panniculitis. J. Am. Acad. Dermatol. 2001, 45, 163–183; quiz 184. [Google Scholar] [CrossRef] [PubMed]
- Thurber, S.; Kohler, S. Histopathologic spectrum of erythema nodosum. J. Cutan. Pathol. 2006, 33, 18–26. [Google Scholar] [CrossRef]
- Mössner, R.; Zimmer, L.; Berking, C.; Hoeller, C.; Loquai, C.; Richtig, E.; Kähler, K.C.; Hassel, J.C.; Gutzmer, R.; Ugurel, S. Erythema nodosum-like lesions during BRAF inhibitor therapy: Report on 16 new cases and review of the literature. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 1797–1806. [Google Scholar] [CrossRef] [PubMed]
- De Simone, C.; Caldarola, G.; Scaldaferri, F.; Petito, V.; Perino, F.; Arena, V.; Papini, M.; Caproni, M.; Peris, K. Clinical, histopathological, and immunological evaluation of a series of patients with erythema nodosum. Int. J. Dermatol. 2016, 55, e289–e294. [Google Scholar] [CrossRef]
- Requena, L.; Yus, E.S. Erythema nodosum. Dermatol. Clin. 2008, 26, 425–438. [Google Scholar] [CrossRef] [PubMed]
- Lazaridou, E.; Apalla, Z.; Patsatsi, A.; Trigoni, A.; Ioannides, D. Erythema nodosum migrans in a male patient with hepatitis B infection. Clin. Exp. Dermatol. 2009, 34, 497–499. [Google Scholar] [CrossRef] [PubMed]
- Inamadar, A.C.; Adya, K.A. The rash with painful and erythematous nodules. Clin. Dermatol. 2019, 37, 129–135. [Google Scholar] [CrossRef]
- Dogan, S.; Karaduman, A.; Evans, S.E. Clinical and laboratory characteristics of patients with erythema nodosum. Skinmed 2016, 14, 99–103. [Google Scholar] [PubMed]
- Chowaniec, M.; Starba, A.; Wiland, P. Erythema nodosum—review of the literature. Reumatologia 2016, 54, 79–82. [Google Scholar] [CrossRef] [PubMed]
- James, W.D.; Berger, T.G.; Elston, D.M. Diseases of subcutaneous fat. In Andrews’ Diseases of the Skin Clinical Dermatology, 12th ed.; Elsevier: Philadelphia, PA, USA, 2016; pp. 480–490. [Google Scholar]
- Gilchrist, H.; Patterson, J.W. Erythema nodosum and erythema induratum (nodular vasculitis): Diagnosis and management. Dermatol. Ther. 2010, 23, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Song, J.S.; Halim, K.; Vleugels, R.A.; Merola, J.F. Dapsone for treatment of erythema nodosum. Dermatol. Online J. 2016, 22. [Google Scholar] [CrossRef]
- Dastoli, S.; Nisticò, S.P.; Morrone, P.; Patruno, C.; Leo, A.; Citraro, R.; Gallelli, L.; Russo, E.; De Sarro, G.; Bennardo, L. Colchicine in managing skin conditions: A systematic review. Pharmaceutics 2022, 14, 294. [Google Scholar] [CrossRef] [PubMed]
- Spagnuolo, R.; Dastoli, S.; Silvestri, M.; Cosco, C.; Garieri, P.; Bennardo, L.; Nisticò, S.P. Anti-interleukin 12/23 in the treatment of erythema nodosum and Crohn disease: A case report. Dermatol. Ther. 2019, 32, e12811. [Google Scholar] [CrossRef] [PubMed]
- Hanzel, J.; Ma, C.; Casteele, N.V.; Khanna, R.; Jairath, V.; Feagan, B.G. Vedolizumab and extraintestinal manifestations in inflammatory bowel disease. Drugs 2021, 81, 333–347. [Google Scholar] [CrossRef] [PubMed]
- Moraes, A.J.P.; Soares, P.M.F.; Zapata, A.L.; Lotito, A.P.N.; Sallum, A.M.E.; Silva, C.A.A. Panniculitis in childhood and adolescence. Pediatr. Int. 2006, 48, 48–53. [Google Scholar] [CrossRef] [PubMed]

| Primary | Idiopathic | ||
|---|---|---|---|
| Secondary | Infectious | Bacterial | |
| Fungal | |||
| Viral | |||
| Protozoal | |||
| Systemic | Sarcoidosis | ||
| IBD: CD, UC | |||
| Behçet Disease | |||
| Sjogren Disease | |||
| Celiac Disease | |||
| Autoimmune Hepatitis | |||
| Spondiloarthropathy | |||
| Vasculitis: Kawasaki, Takayasu | |||
| Monogenic Autoinflammatory Diseases: Blau Syndrome, CAPS, HIDS | |||
| Sweet syndrome | |||
| Malignancy | Lymphoprolipherative: Leukemia, Lymphoma (Hodgkin and non-Hodgkin) Solid Tumors: Carcinoid, Sarcoma | ||
| Others | Drugs: Antibiotics (Penicillin, Macrolides, Cephalosporin), PPI, Everolimus, Aspirin, Contraceptives, Azathioprine, Phenitoin, Valproate | ||
| Vaccination: BCG, DTaP, HPV, SARS-CoV-2 | |||
| Labbé 1996 [5] | Kakourou 2001 [7] | Hassink 1997 [10] | Garty 2000 [14] | Aydın-Teke 2014 [11] | Litwin 2014 [15] | Picco 1999 [12] | Cengiz 2006 [13] | |
|---|---|---|---|---|---|---|---|---|
| N° tot cases | 27 | 35 | 36 | 24 | 39 | 12 | 22 | 10 |
| M/F | 15/12 | 17/18 | 18/18 | 8/16 | 18/21 | 5/7 | 12/10 | 5/5 |
| Mean age, yrs. | 9 | 8.9 | 10 | 9.9 | 11.3 | 11.9 | 10.4 | 8.8 |
| Idiopathic, % | 41 | 23 | 22 | 33 | 44 | 25 | 27.2 | 50 |
| Secondary, % | 59 | 77 | 78 | 67 | 56 | 75 | 72.7 | 50 |
| Infectious, % | 55 | 71 | 55 | 46 | 51 | 50 | 45.4 | 50 |
| GAS | 22 | 48 | 27 | 25 | 22 | 25 | 22.7 | 30 |
| TB | 5.7 | 7.5 | 4.5 | 20 | ||||
| RTI | 11 | 8.5 | 13.8 | 5.5 | 8.3 | |||
| GI | 22 | 8.5 | 8.3 | 2.5 | 8.3 | 4.5 | ||
| Cat scratch | 4 | |||||||
| EBV | 2.7 | 17 | 4.5 | |||||
| CMV | 2.5 | |||||||
| HPV-B19 | 2.7 | |||||||
| Tularemia | 10.2 | |||||||
| Other | 8.3 | |||||||
| Sarcoidosis | 4 | 2.7 | 2.5 | |||||
| IBD | 2.8 | 16.6 | 13 | 25 | 13.6 | |||
| Behçet | 2.7 | 8 | 2.5 | 9 | ||||
| Malignancy | 2.8 | |||||||
| SpA | 9 |
| Bacterial | Viral | Fungal | Protozoal |
|---|---|---|---|
| GAS | EBV | Candida albicans | Giardia lamblia |
| Mycobacterium tuberculosis | HBV | Trichophyton mentagrophytes | Entamoeba histolytica |
| Atypical mycobacteria | HCV | Coccidioides immitis | Toxoplasma gondii |
| Yersinia enterocolitica | HPV B19 | Blastomices dermatitidis | |
| Salmonella spp. | HIV | Histoplasma capsulatum | |
| Campylobacter jejuni | CMV | Sporothrix schenckii | |
| Mycoplasma pneumoniae | Parapoxvirus | ||
| Chlamydia trachomatis | VZV | ||
| Chlamydia psittaci | SARS-CoV-2 | ||
| Coxiella burneti | |||
| Bartonella henselae | |||
| Helicobacter pylori | |||
| Gardnerella vaginalis | y | ||
| Francisella tularensis | |||
| Leptospira | |||
| Brucella spp. | |||
| Shigella flexneri | |||
| Burkholderia pseudomallei |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trapani, S.; Rubino, C.; Lodi, L.; Resti, M.; Indolfi, G. Erythema Nodosum in Children: A Narrative Review and a Practical Approach. Children 2022, 9, 511. https://doi.org/10.3390/children9040511
Trapani S, Rubino C, Lodi L, Resti M, Indolfi G. Erythema Nodosum in Children: A Narrative Review and a Practical Approach. Children. 2022; 9(4):511. https://doi.org/10.3390/children9040511
Chicago/Turabian StyleTrapani, Sandra, Chiara Rubino, Lorenzo Lodi, Massimo Resti, and Giuseppe Indolfi. 2022. "Erythema Nodosum in Children: A Narrative Review and a Practical Approach" Children 9, no. 4: 511. https://doi.org/10.3390/children9040511