Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Immunofluorescence description | Immunofluorescence images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mintline M, Smith MH. Lichen planus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavitylichenplanus.html. Accessed May 6th, 2024.
Definition / general
- Chronic, T cell mediated inflammatory mucocutaneous disorder of uncertain etiology and pathogenesis
- Characterized by relapses and remissions
Essential features
- Common oral mucosal disease with multifocal, bilateral and symmetrical involvement
- Characterized by white, lace-like lesions (Wickham striae) with or without atrophic or erosive areas
- Accurate identification is challenging and often requires clinicopathological correlation
- Histopathology is nonspecific but includes hyperkeratosis, interface mucositis, hydropic degeneration and apoptotic keratinocytes
- Direct immunofluorescence is nonspecific with a shaggy deposition of fibrinogen at the basement membrane zone
Terminology
- Lichen planus
ICD coding
Epidemiology
- Global oral lichen planus prevalence is 1.01% (Oral Dis 2021;27:813)
- Most commonly seen in middle aged adults (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:S25.e1)
- Rarely seen in pediatric populations (Pediatr Dermatol 2014;31:59)
- F > M (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:S25.e1)
- May be associated with hepatitis C (varies geographically) (Br J Dermatol 2004;151:1172)
Sites
- Intraoral
- Oral lichen planus is typically multifocal and bilateral with a symmetric distribution of lesions
- Most common site is buccal mucosa; oral lichen planus usually involves the buccal mucosa bilaterally
- May affect the gingiva, vestibule and labial mucosa; tongue involvement is uncommon (J Cancer Prev 2016;21:55)
- Extraoral
- Skin (flexor, wrists and forearms, dorsal hands, shins, presacral area), mucous membranes (oral mucosa, genitalia), hair, nails, esophagus (rare)
- 16% of oral lichen planus patients also have cutaneous involvement (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:431)
Pathophysiology
- Unknown pathogenesis (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:72)
Etiology
- Believed to be a T cell mediated chronic inflammatory oral mucosal disease of unknown etiology (J Oral Pathol Med 2010;39:729)
Clinical features
- Most common clinical patterns of oral lichen planus are the reticular and erosive forms (Head Neck Pathol 2020;14:192)
- Reticular pattern: characterized by thin, interlacing and white lines (Wickham striae); lesions typically wax and wane over weeks or months (Oral Maxillofac Surg Clin North Am 2013;25:93)
- Erosive pattern: characterized by atrophic and erythematous areas with central ulceration
- Other clinical patterns include atrophic, papular, plaque and bullous forms (Clin Dermatol 2016;34:495)
- Reactive pigmentation may be seen, particularly in persons of color (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332)
- Multiple forms may be seen in one patient; clinical forms represent the same disease process
- Worse symptoms / lesions tend to be in areas of trauma, chronic irritation, poor oral hygiene
Diagnosis
- Diagnosis is based on both clinical and histopathologic features (J Oral Pathol Med 2021;50:520)
- Histopathologic features of oral lichen planus may mimic numerous pathologic processes with an inflammatory infiltrate (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332)
- Adjunct direct immunofluorescence may be beneficial to differentiate oral lichen planus from conditions with similar histomorphology (e.g., chronic ulcerative stomatitis) or clinical features (e.g., mucous membrane pemphigoid and pemphigus vulgaris) (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332)
- Direct immunofluorescence does not distinguish lichen planus from oral dysplasia (Oral Surg Oral Med Oral Pathol Oral Radiol 2015;119:675)
Prognostic factors
- Oral lichen planus is characterized by relapses and remissions
- Uncertain malignant potential
- Small subset of patients with oral lichen planus (1.1%) develops oral squamous cell carcinoma (Oral Oncol 2017;68:92)
Case reports
- 8 year old boy with oral ulcerations (J Oral Maxillofac Pathol 2020;24:S128)
- 57 year old man with bilateral white lesions of the buccal mucosa (Head Neck Pathol 2020;14:192)
- 77 year old woman with desquamative gingivitis (Case Rep Dent 2019;2019:4659134)
Treatment
- Reticular oral lichen planus is often asymptomatic; no treatment is needed, although management includes monitoring patients at regular intervals to ensure the lesions are migrating or changing patterns
- Photographic documentation is beneficial (Head Neck Pathol 2019;13:423)
- Lesions that do not migrate are concerning for evolving oral dysplasia or contact related lichenoid lesions
- Erosive oral lichen planus is often bothersome due to open sores; typically managed with topical or systemic corticosteroids (Cochrane Database Syst Rev 2020;2:CD001168)
Clinical images
Gross description
- Nonspecific
- Often tan wedge of mucosa with white striations, papules, erosions or ulcerations
Microscopic (histologic) description
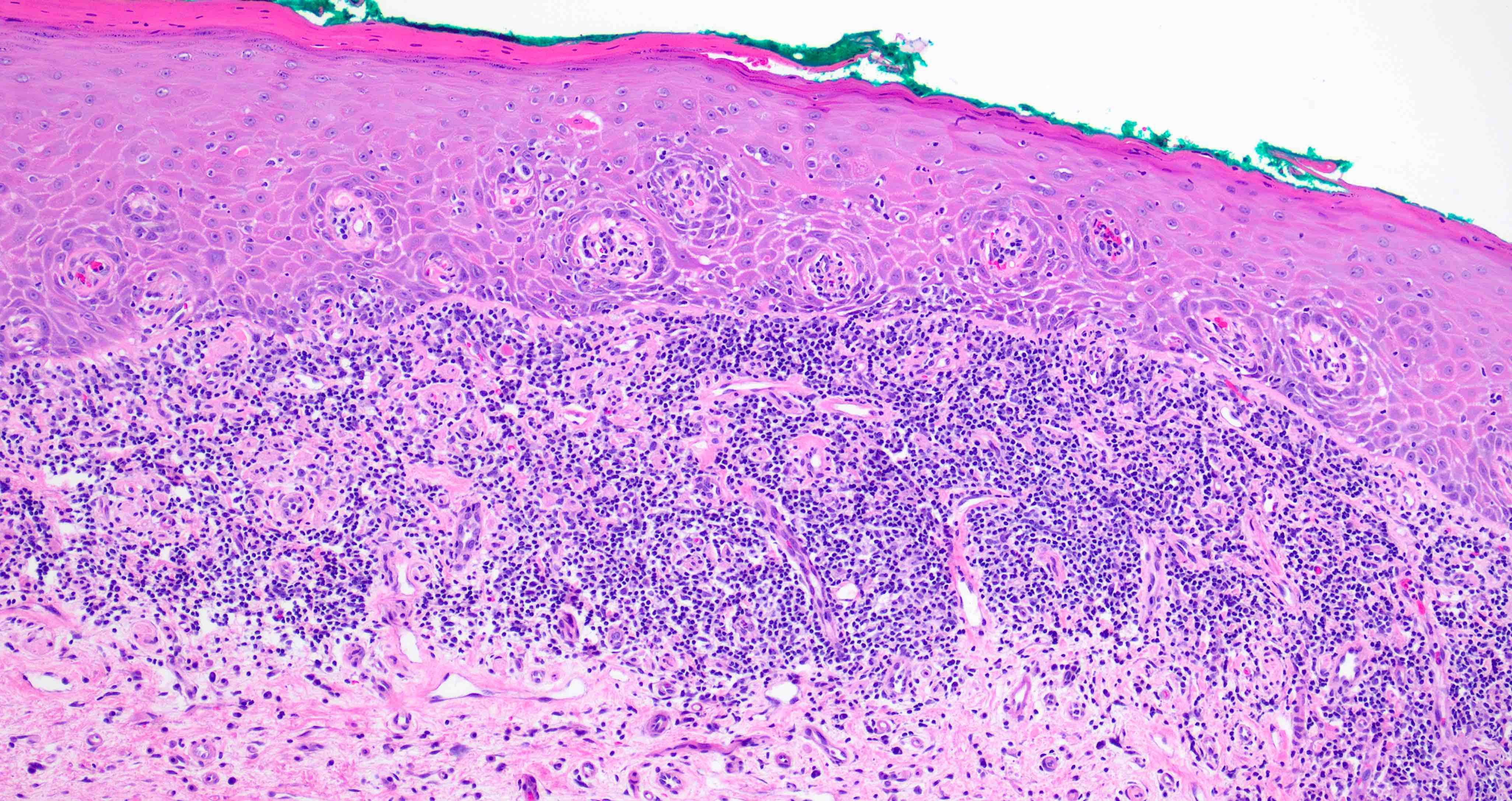
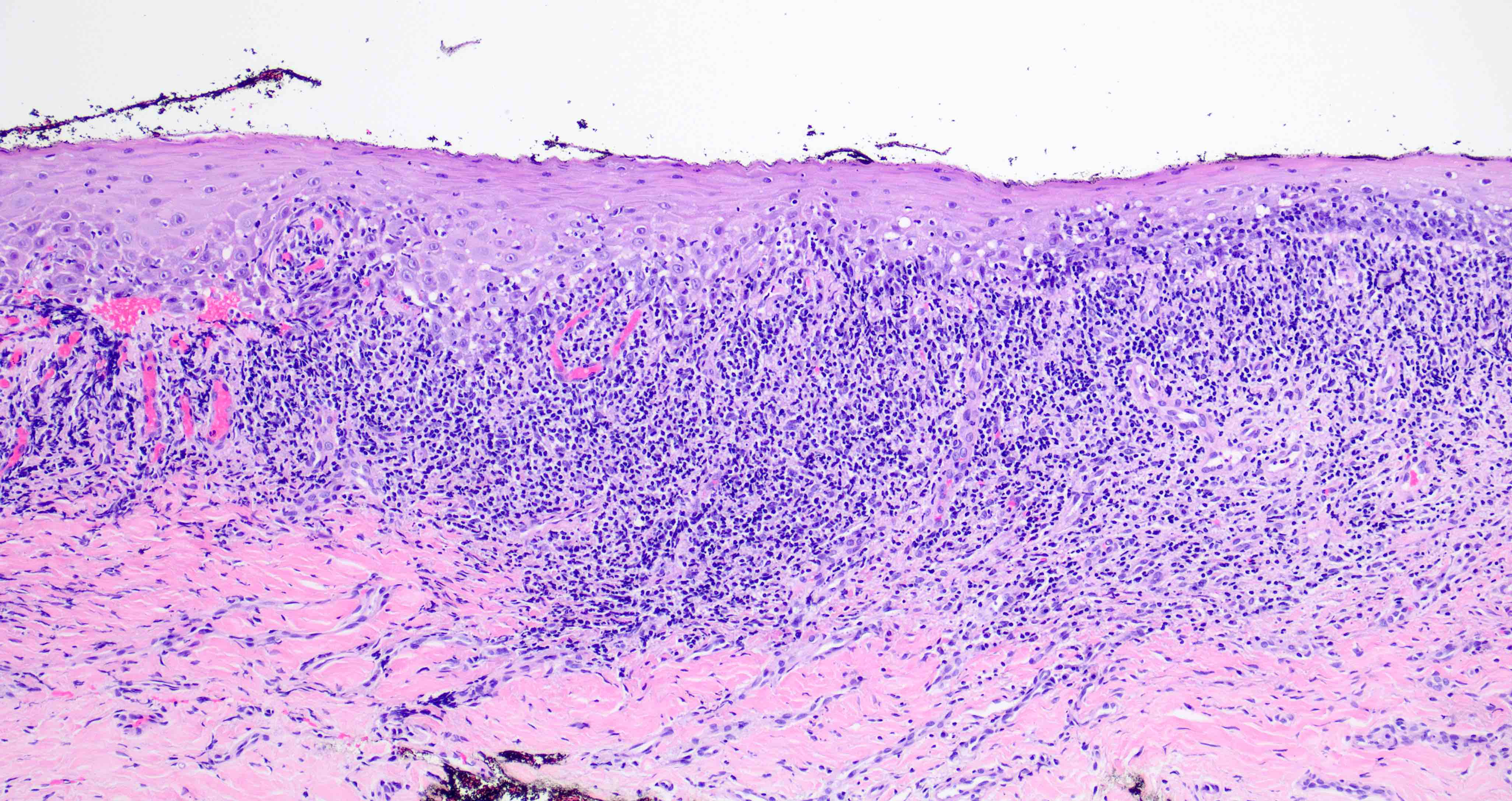
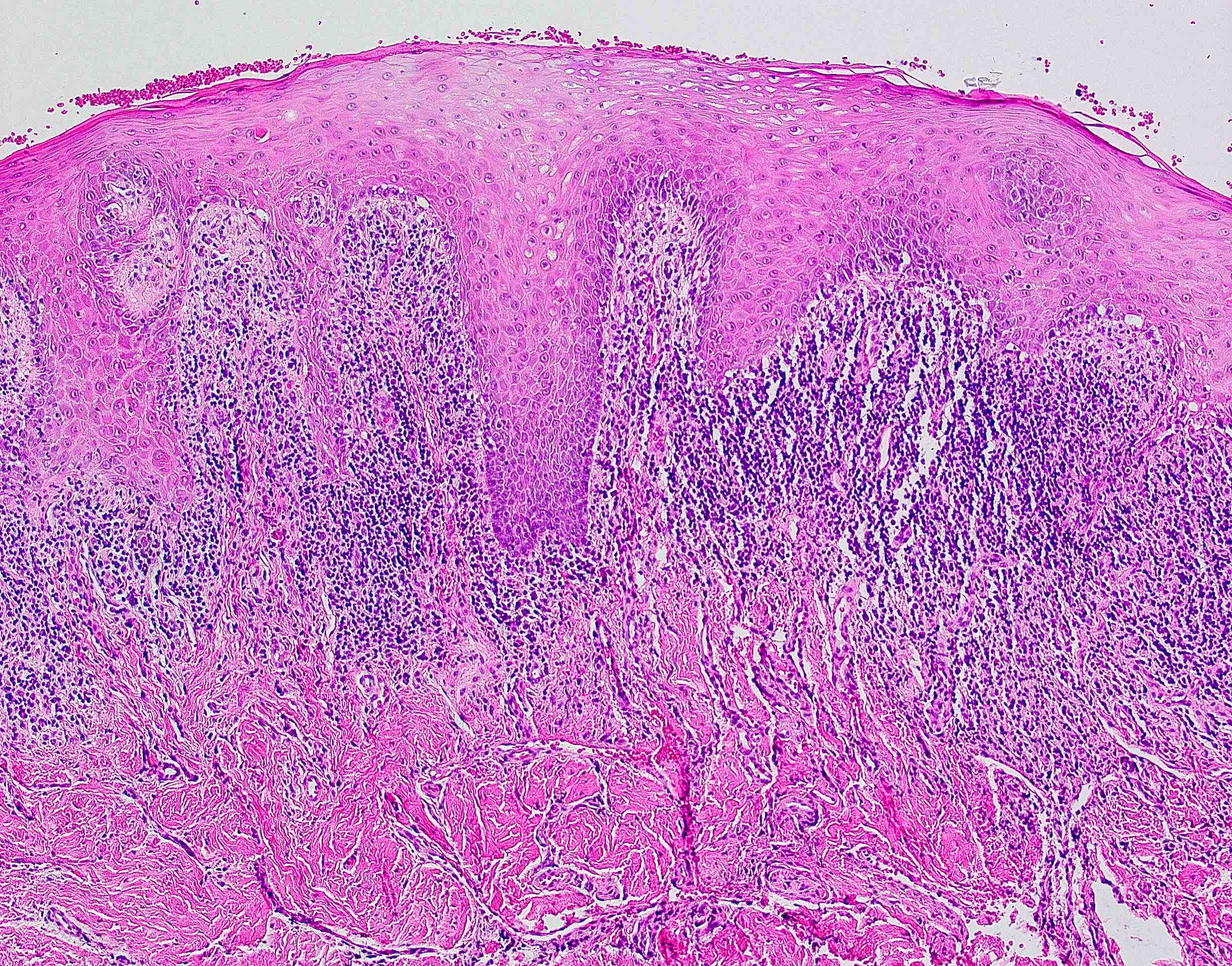
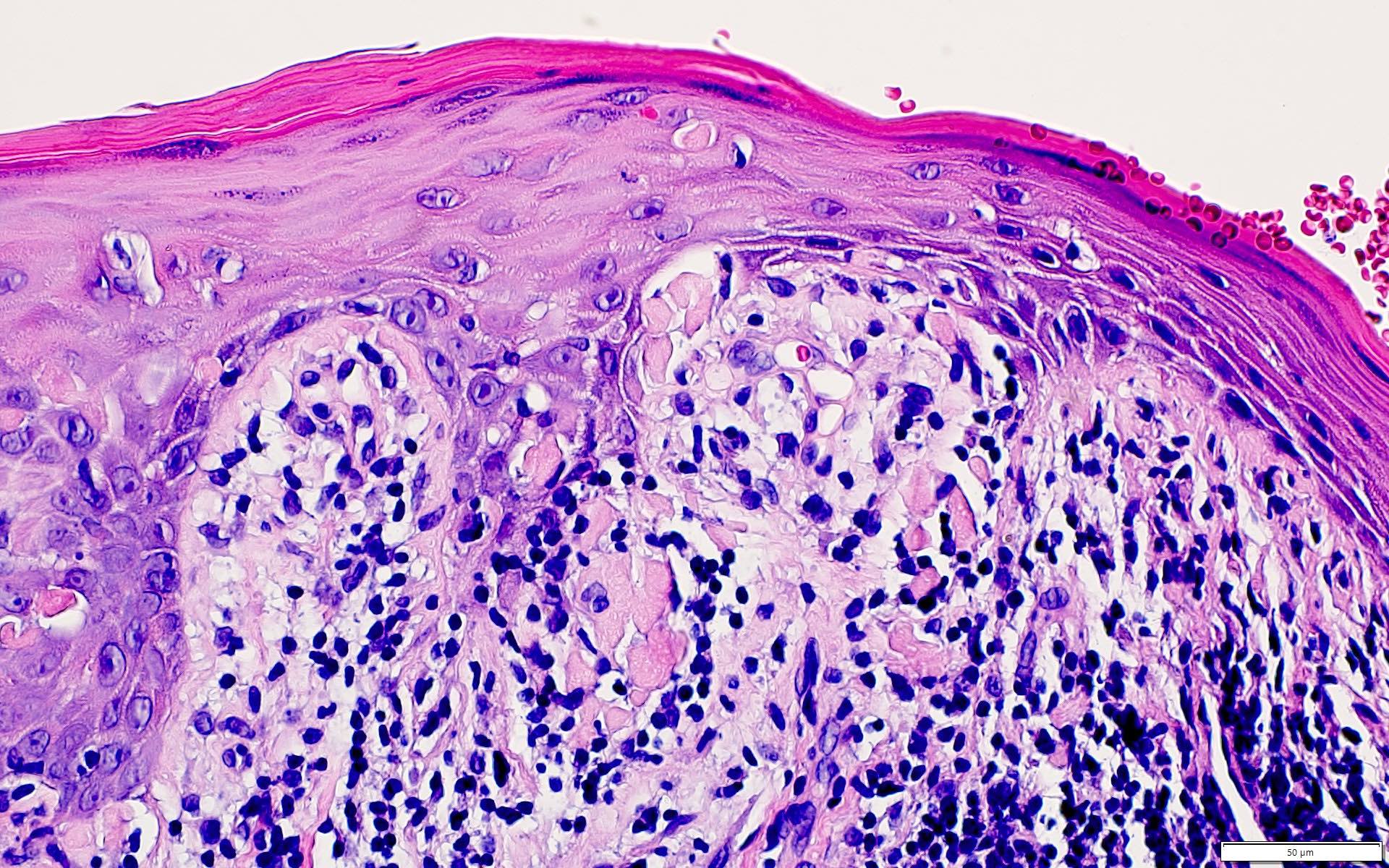
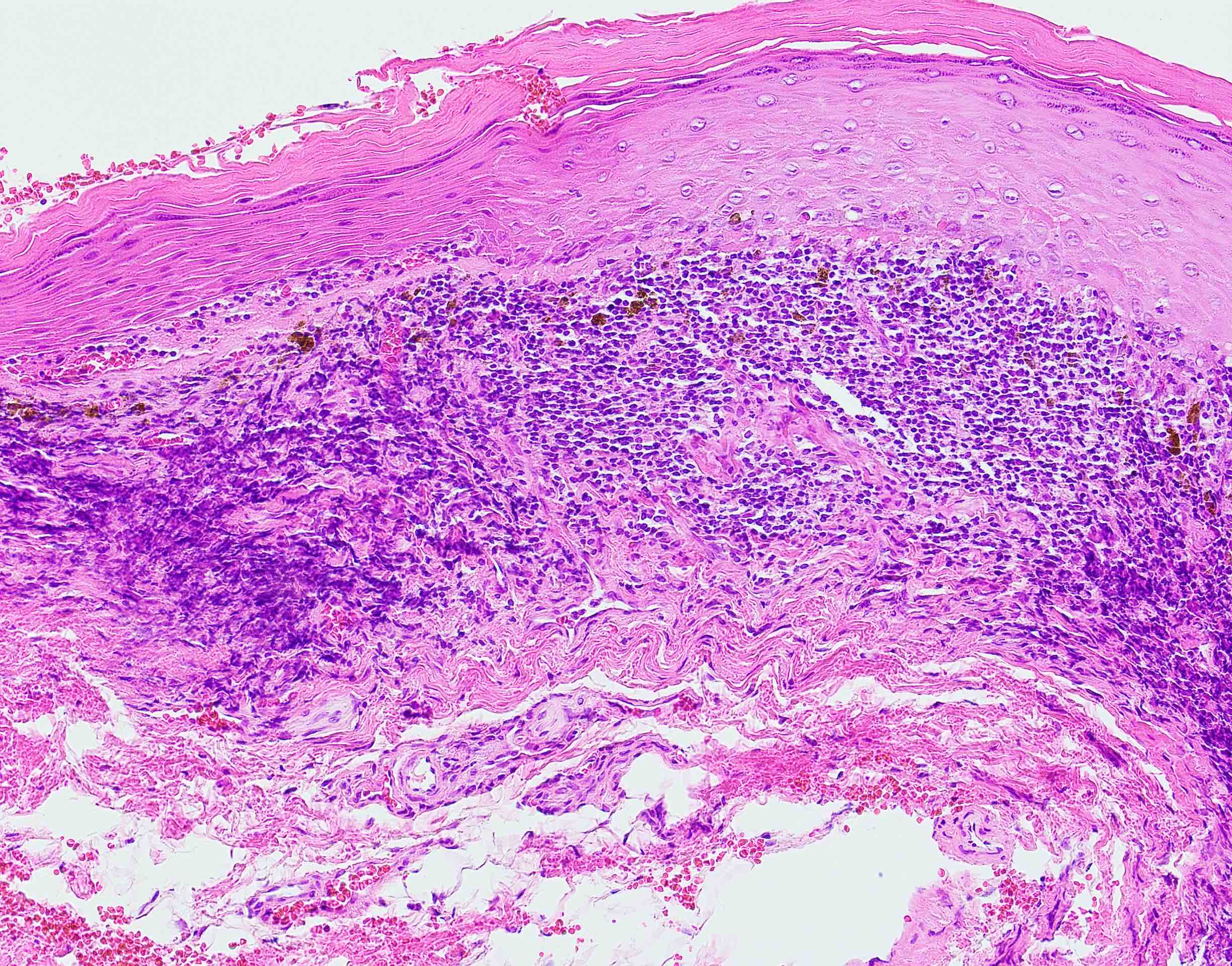
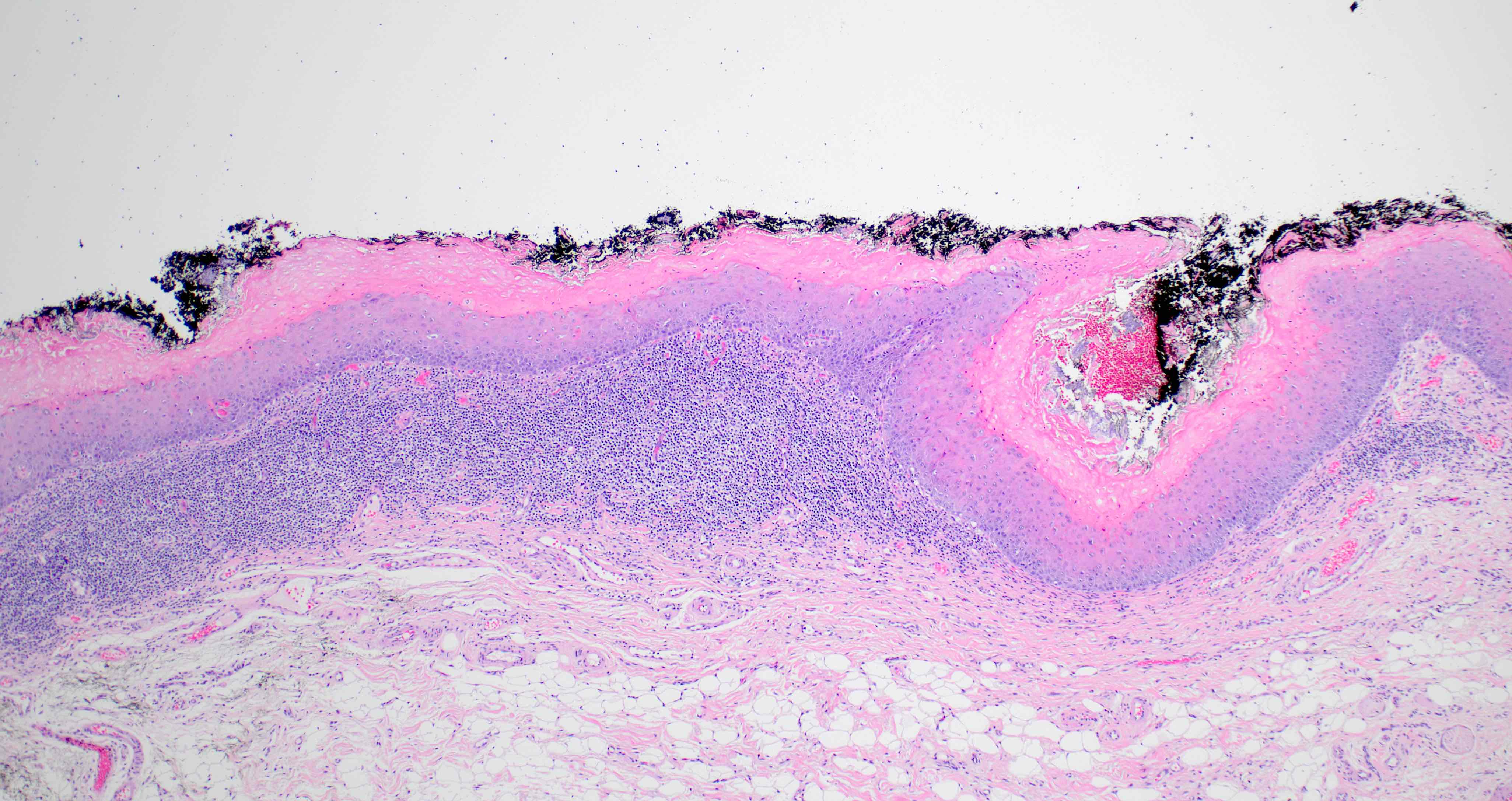
- 2003 modified WHO criteria may have more specificity than the 1978 WHO criteria (Int J Prev Med 2021;12:126, J Oral Pathol Med 2003;32:507):
- Orthokeratosis or parakeratosis
- Epithelial thickness varies, sawtooth rete ridges occasionally seen
- Colloid (civatte) bodies in the epithelium or superficial lamina propria
- Thin band of eosinophilic material in the basement membrane
- Well defined, band-like zone of cellular infiltration consisting mainly of lymphocytes and confined to the superficial lamina propria
- Liquefactive degeneration in the basal cell layer (hydropic degeneration)
- Absence of epithelial dysplasia
- Additional criteria proposed by Cheng et al. 2016 (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332):
- Band-like or patchy, predominantly lymphocytic infiltrate in the lamina propria that is confined to the interface of the epithelium and lamina propria
- Lymphocytic exocytosis
- Absence of epithelial dysplasia
- Absence of verrucous epithelial architectural changes
- Histopathologic features of oral lichen planus are nonspecific and should be correlated with clinical features (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332)
Microscopic (histologic) images
Immunofluorescence description
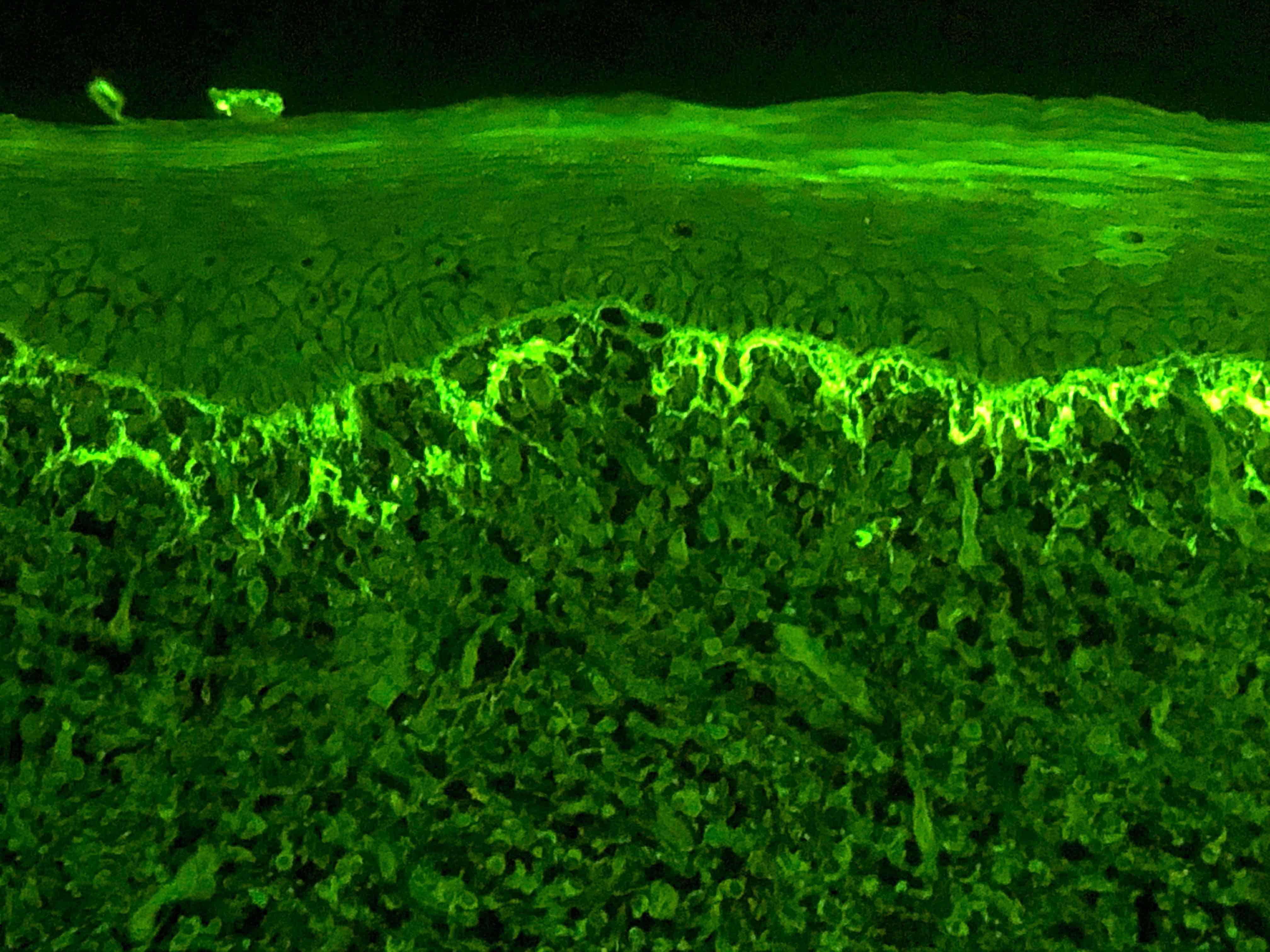
- Direct immunofluorescence is nonspecific
- IgG, IgA, IgM and complement (C3) are characteristically negative
- Shaggy, linear deposition of fibrinogen may be seen at the basement membrane zone
- Fibrinogen positivity at the basement membrane zone may also be seen in epithelial dysplasia and squamous cell carcinoma (Oral Surg Oral Med Oral Pathol Oral Radiol 2015;119:675)
- Colloid bodies may be positive for immunoglobulins
- Indirect immunofluorescence is negative
Positive stains
- PAS (colloid bodies)
Sample pathology report
- Buccal mucosa, incisional biopsy:
- Chronic interface mucositis and hyperparakeratosis (see comment)
- Comment: The histomorphology of interface mucositis combined with the clinical presentation of bilateral, migrating erosions with Wickham striae is most consistent with oral lichen planus.
Differential diagnosis
- Oral lichenoid drug reaction:
- Oral mucosal immunoinflammatory disorder characterized by erythematous plaques, vesiculation, ulceration or hyperkeratosis in response to a medication (Dermatol Ther 2010;23:251)
- Time range between initiation of medication and onset of reaction can vary widely
- Resembles oral lichen planus; mixed inflammation may extend into the deep lamina propria, may show perivascular inflammation
- Epithelium may have a greater number of colloid bodies (Int J Dermatol 2012;51:1199)
- Infiltrate may be more diffuse or mixed with plasma cells
- Indirect immunofluorescence may detect circulating antibodies directed to basal cells in a string of pearls pattern (Am J Dermatopathol 1982;4:155)
- Common implicated medications: nonsteroidal anti-inflammatory drugs, anticonvulsants, antihypertensives, antimalarials and antiretrovirals
- Oral lichenoid contact hypersensitivity reaction:
- Oral mucosal immunoinflammatory disorder characterized by erythematous plaques, vesiculation, ulceration or hyperkeratosis in response to a local agent (Oral Surg Oral Med Oral Pathol Oral Radiol 2017;123:559)
- May present with pain, burning sensation or itchiness (Oral Surg Oral Med Oral Pathol Oral Radiol 2017;123:559)
- Lichenoid interface mucositis; mixed inflammation may extend into the deep lamina propria, may show perivascular inflammation (Eur J Dermatol 2004;14:284)
- Common implicated agents: mouthwashes, foods, spices (particularly cinnamon), gloves, rubber dams and dental materials (Eur J Dermatol 2004;14:284)
- Chronic ulcerative stomatitis:
- Rare, autoimmune disorder that affects the oral mucosa (J Oral Pathol Med 2022;51:501)
- Patients develop autoantibodies against nuclear protein ΔNp63α (an isoform of p63) (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;111:742)
- Clinically, lesions often respond to antimalarial medications and are less responsive to corticosteroid therapy than oral lichen planus (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332, Oral Dis 2008;14:383)
- Histopathological features may be indistinguishable from oral lichen planus; often demonstrates marked epithelial atrophy (Head Neck Pathol 2019;13:386)
- Direct immunofluorescence: specific antinuclear antibody (SES ANA) pattern; IgG antibodies present in the nuclei of basal and parabasal cells (Head Neck Pathol 2019;13:386)
- Oral graft versus host disease:
- Clinical and histopathological presentations are similar to oral lichen planus
- Develops as a result of allogeneic hematopoietic cell transplantation
- Lupus erythematosus:
- Oral involvement in ~25% of cases (Expert Rev Mol Diagn 2014;14:169)
- Majority of cases have cutaneous involvement or systemic inflammatory disease
- Histopathology resembles oral lichen planus; may have perivascular inflammation
- Direct immunofluorescence: linear band or continuous granular IgG, IgM, IgA or C3 at the basement membrane zone
- Proliferative verrucous leukoplakia:
- Multifocal, aggressive form of oral leukoplakia with a tendency to recur and undergo malignant transformation (Head Neck 2014;36:1662)
- Clinicopathological diagnosis (Head Neck Pathol 2021;15:572)
- Early lesions may mimic oral lichen planus clinically and microscopically
- Histopathology may have inflammatory infiltrate (Head Neck Pathol 2021;15:572)
- Oral lichen planus should lack a prominent corrugated architecture (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332)
- Evolving / early dysplasia:
- Clinical correlation is necessary to distinguish from oral lichen planus
- Oral dysplastic lesions may demonstrate lichenoid inflammatory infiltrate in superficial lamina propria
- Clinically, the lesion does not migrate or change patterns
- Foreign body gingivitis:
- White, progressing, verrucous / corrugated clinical lesions (mimicking proliferative verrucous leukoplakia) were recently found to be strongly associated with granules of embedded foreign material (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:250)
- Similar histomorphology to oral lichen planus; however, inflammatory infiltrate is often mixed and patchy, containing minuscule granules of foreign material
- Silica is the most common element found in the embedded foreign material (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:250)
Board review style question #1
A 54 year old woman presents to her dentist for a routine examination. Clinical examination reveals thin, interlacing white lines on the buccal mucosa. The lesions present bilaterally. The patient reports that the lesions are asymptomatic and that she had them for years. She reports that the lesions tend to wax and wane. What is the most likely diagnosis?
- Lichen planus
- Mucous membrane pemphigoid
- Oral candidiasis
- Pemphigus vulgaris
- Squamous cell carcinoma
Board review style answer #1
A. Lichen planus. The prevalence of oral lichen planus is 0.1% to 2.2%. The 2 most common clinical patterns of oral lichen planus are reticular and erosive. Reticular oral lichen planus is named because of its characteristic pattern of interlacing white lines (Wickham striae).
Comment Here
Reference: Lichen planus
Comment Here
Reference: Lichen planus
Board review style question #2
Which direct immunofluorescence finding is most supportive of oral lichen planus?
- IgG in the basal and parabasal epithelial nuclei
- Intracellular IgG deposition
- Linear IgG deposition at the basement membrane zone
- Shaggy, linear deposition of fibrinogen at the basement membrane zone
Board review style answer #2
D. Shaggy, linear deposition of fibrinogen at the basement membrane zone. Direct immunofluorescence studies may be necessary to differentiate oral lichen planus from autoimmune blistering diseases. Shaggy deposition of fibrinogen at the basement membrane zone and the absence of immunoglobulin is seen in oral lichen planus.
Comment Here
Reference: Lichen planus
Comment Here
Reference: Lichen planus