Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Smith MH. Parulis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavityparulis.html. Accessed May 5th, 2024.
Definition / general
- Localized collection of acute inflammation and edematous granulation tissue on the gingiva, which represents the intraoral opening of a draining odontogenic (dental) infection
Essential features
- Reactive soft tissue swelling of the gingiva
- By definition, must be associated with draining dental abscess / infection (periapical or periodontal fistula)
- Similar to pyogenic granuloma but contains linear tracks or accumulations of neutrophils
- Must treat the source of infection, since surgical removal of the parulis alone likely will lead to recurrence
Terminology
- Gum boil
- Dental fistulous tract / dental fistula
- Dental abscess with sinus tract
ICD coding
- ICD-10: K04.6 - periapical abscess with sinus
Sites
- Exclusively occurs on the gingiva; attached or unattached gingiva
Etiology
- Associated with dental infection
- Pulpal necrosis, abscess (Eur Endod J 2020;5:54)
- Infection associated with an untreated dental cavity
- Infection surrounding dental implant, embedded foreign material or other oral prosthesis
Clinical features
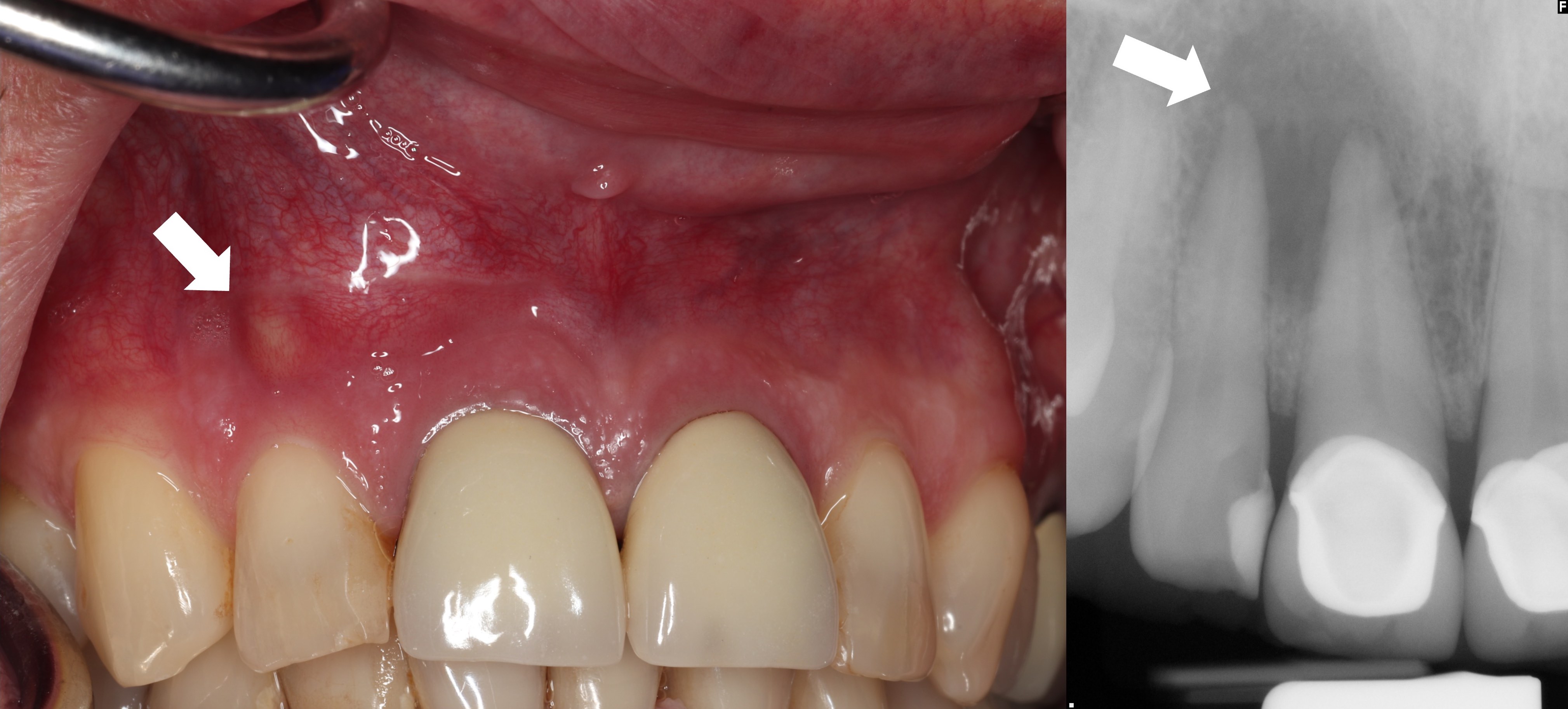
- Smooth and sometimes lobulated exophytic polypoid lesion on the gingiva
- Yellow, red or pink (when fibrosed) in color (Case Rep Dent 2018;2018:4850901)
- Often fluctuant
- Light pressure may reveal drainage of purulent exudate
Diagnosis
- Diagnosis is most often made upon clinical evaluation of fluctuant / draining gingival nodule associated with adjacent dental infection; histopathologic confirmation is useful but may not be needed
- Pulpal necrosis is evaluated with electric pulp testing or thermal evaluation in combination with radiographic correlation
- Intraoral sinus track can be traced with gutta percha to help confirm etiologic origin (J Clin Diagn Res 2013;7:2392)
Radiology description
- Parulides may be accompanied by an ill or well defined radiolucency at or around the apex of a nonvital tooth (Eur Endod J 2020;5:54)
Case reports
- 40 year old woman with multiple parulides (intraoral draining sinus tracts) all associated with a single necrotic tooth (J Clin Diagn Res 2013;7:2392)
- 53 year old woman with parulis forming around dental implant (J Oral Implantol 2016;42:505)
- 59 year old man presents with a large exophytic mass of the gingiva adjacent to a necrotic tooth (Case Rep Dent 2018;2018:4850901)
Treatment
- While the gingival nodule may be removed surgically, the nodule will recur without effective treatment of the underlying associated infection (e.g., root canal therapy, dental extraction, etc.) (Eur Endod J 2020;5:54)
- Antibiotics not indicated unless systemic spread is present (Fertil Steril 1986;45:75)
Clinical images
Gross description
- Tan / gray / brown nodule that often collapses upon sectioning and contains yellow exudate
Microscopic (histologic) description
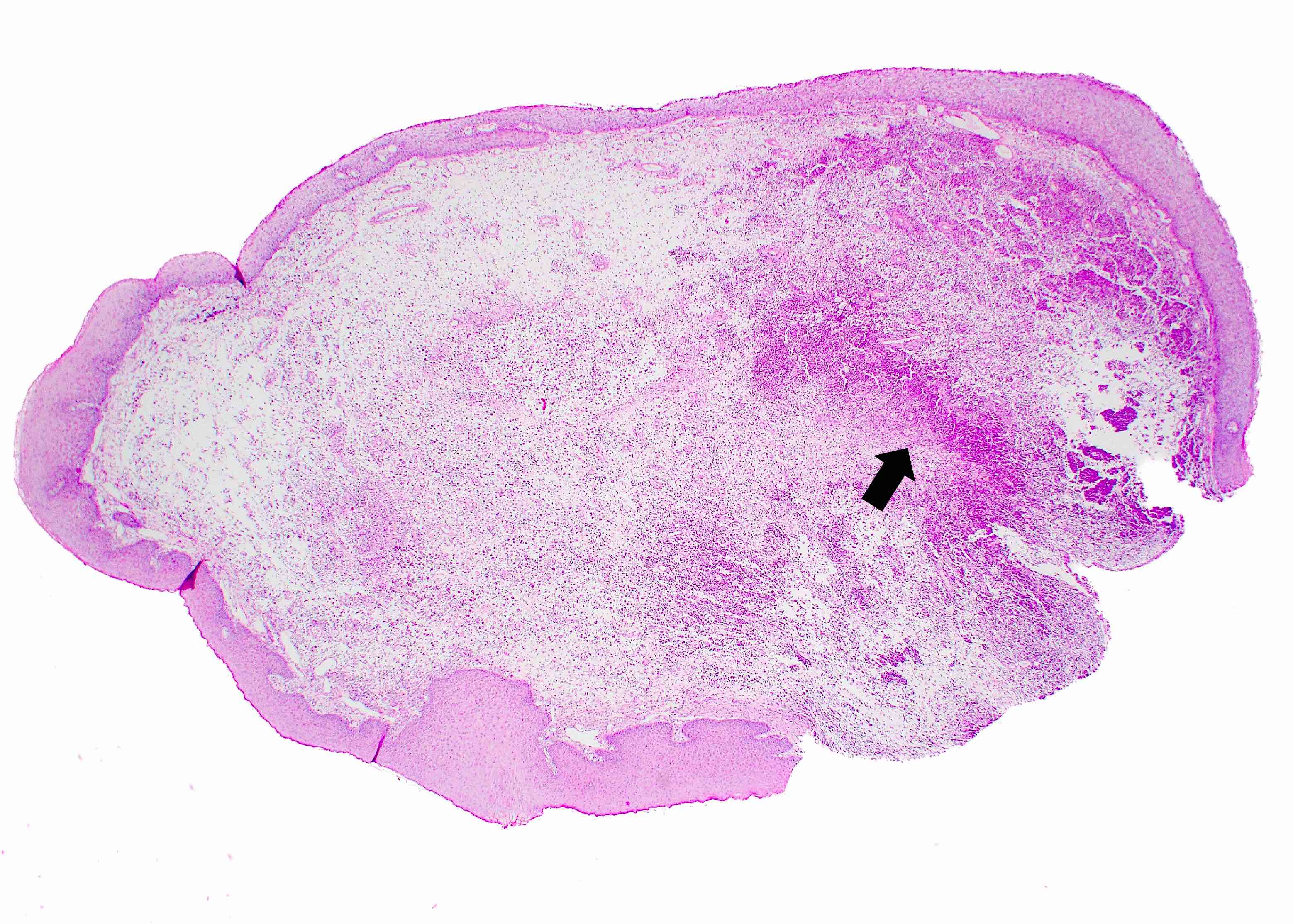
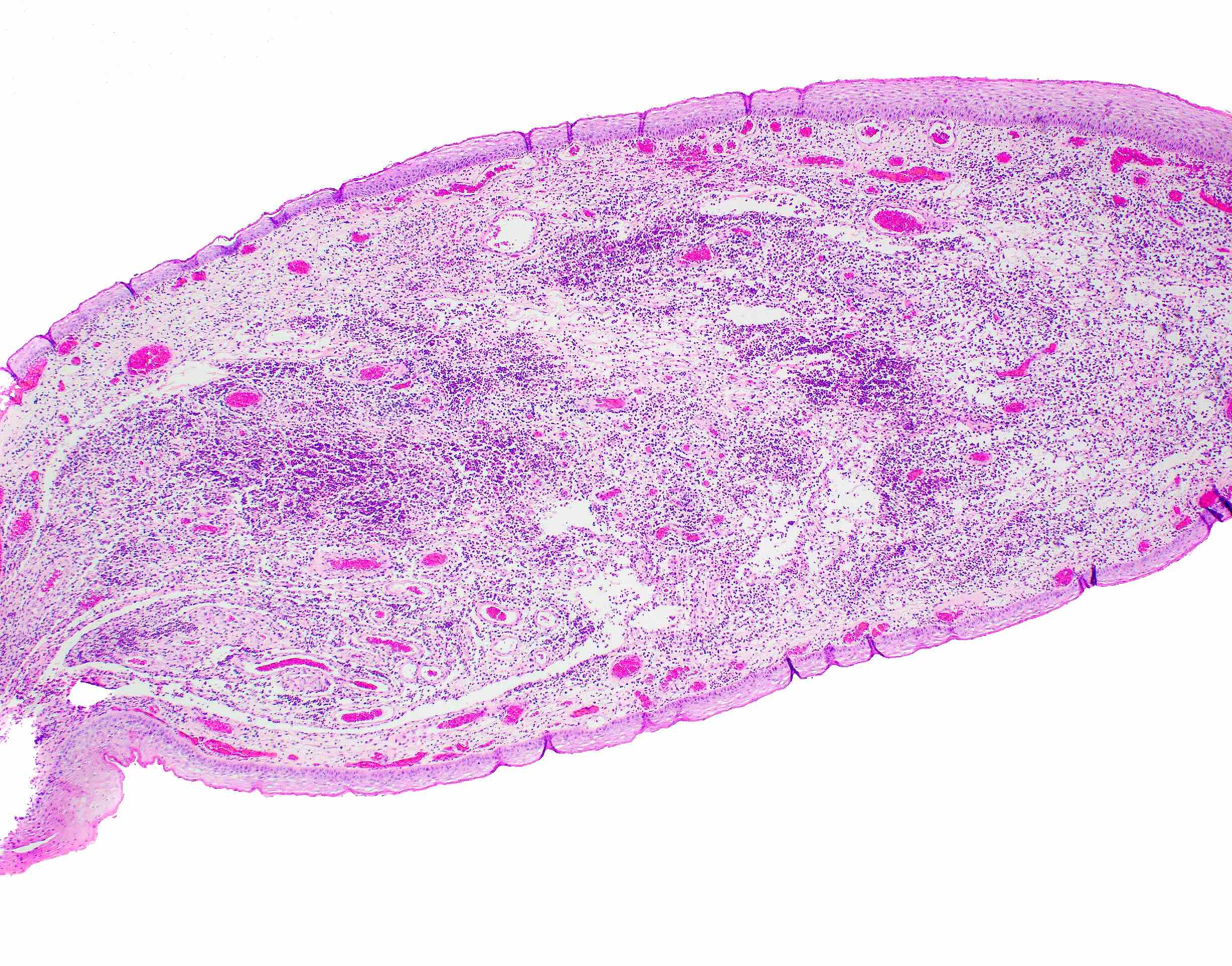
- Nodule or collapsed nodule surfaced by keratinized squamous epithelium and comprised of edematous granulation tissue (World J Clin Cases 2015;3:779)
- Collections or linear tracts of neutrophils are present and often extend to the base of the specimen
Microscopic (histologic) images
Videos
Etiology and treatment of a dental fistulous tract / parulis
Tracing a dental fistulous tract with gutta percha
Sample pathology report
- Gingiva, excisional biopsy:
- Granulation tissue with linear tracts of neutrophils (see comment)
- Comment: When combined with the clinical information, the histomorphology is compatible with a parulis (draining fistulous tract).
Differential diagnosis
- Histopathologic:
- Pyogenic granuloma:
- May be histopathologically identical / similar, although parulis tends to demonstrate dense accumulations or linear tracts of neutrophils that may extend to the base of the specimen
- Clinical correlation is vital in the differentiation of the two entities
- Distinguishing pyogenic granuloma from parulis is essential for appropriate treatment
- Local excision of the polypoid lesion is sufficient for pyogenic granuloma
- Parulides require treatment of the underlying infection to prevent recurrence
- Pyogenic granuloma:
- Clinical:
- Clinical differential diagnosis for a red, yellow or pink nodule on the gingiva is exhaustive and may include pyogenic granuloma, peripheral giant cell granuloma, peripheral ossifying fibroma, peripheral odontogenic fibroma, localized accumulation of dermal filler, metastatic disease or other malignant or benign tumors (Head Neck Pathol 2019;13:4, World J Clin Cases 2015;3:779, Head Neck Pathol 2013;7:241)
- Identification of a soft tissue gingival nodule, in combination with underlying dental infection, favors diagnosis of parulis
- Excisional biopsy may be used to confirm diagnosis
- Clinical differential diagnosis for a red, yellow or pink nodule on the gingiva is exhaustive and may include pyogenic granuloma, peripheral giant cell granuloma, peripheral ossifying fibroma, peripheral odontogenic fibroma, localized accumulation of dermal filler, metastatic disease or other malignant or benign tumors (Head Neck Pathol 2019;13:4, World J Clin Cases 2015;3:779, Head Neck Pathol 2013;7:241)
Additional references
Board review style question #1
Cone beam computed tomography (CBCT) of the patient shown above demonstrates a well defined, nonexpansile radiolucency surrounding the root of the associated necrotic maxillary incisor. Biopsy shows a nodule of granulation tissue demonstrating dense accumulations of neutrophils at the base of the specimen. What is the most likely diagnosis?
- Foreign body granuloma due to dermal filler
- Leukoplakia
- Parulis
- Pyogenic granuloma
Board review style answer #1
C. Parulis. The main distractor for this gingival nodule comprised of inflamed granulation tissue is a pyogenic granuloma; however, the description of dense accumulations of neutrophils at the base of the specimen favors a parulis, a soft tissue mass representing the intraoral opening of a draining odontogenic (dental) infection. Although both entities are benign, differentiating the two entities is important, as treatment modalities are different.
Although accumulations of dermal filler may present as a yellow nodule in the oral cavity, dermal filler accumulates under unattached mucosa rather than attached gingiva. Past medical history regarding previous cosmetic injections may also aid in excluding this entity from the differential diagnosis.
Leukoplakia is a flat, white patch of the oral cavity and does not clinically present as a nodule or histopathologically as granulation tissue.
Comment Here
Reference: Parulis
Although accumulations of dermal filler may present as a yellow nodule in the oral cavity, dermal filler accumulates under unattached mucosa rather than attached gingiva. Past medical history regarding previous cosmetic injections may also aid in excluding this entity from the differential diagnosis.
Leukoplakia is a flat, white patch of the oral cavity and does not clinically present as a nodule or histopathologically as granulation tissue.
Comment Here
Reference: Parulis
Board review style question #2
Board review style answer #2
A. Parulis. The main distractor for this gingival nodule comprised of inflamed granulation tissue is a pyogenic granuloma; however, the presence of dense accumulations of neutrophils at the base of the specimen favors a parulis, a soft tissue mass representing the intraoral opening of a draining odontogenic (dental) infection. Although both entities are benign, differentiating the two entities is important, as treatment modalities are different.
Peripheral giant cell granulomas contain osteoclast type giant cells, not appreciated within the present biopsy.
Peripheral ossifying fibromas contain focal to large islands of vital bone, not appreciated within this biopsy.
Comment Here
Reference: Parulis
Peripheral giant cell granulomas contain osteoclast type giant cells, not appreciated within the present biopsy.
Peripheral ossifying fibromas contain focal to large islands of vital bone, not appreciated within this biopsy.
Comment Here
Reference: Parulis