Pediatric infectious disease doctor Paul Offit isn’t vaccinated against measles. Like many of his peers, he caught the virus as a child in the 1950s, roughly a decade before a vaccine was created. At that time the highly contagious and potentially fatal disease sickened an estimated three million to four million Americans each year. Offit has been immune ever since and likely will be for life.
For those who haven’t undergone the full-body rash, swollen eyeballs and plethora of other unpleasant symptoms of measles in order to earn a lifelong defense against the disease, the vaccine is key. After widespread adoption of the two-shot vaccine regimen in the 1990s, disease transmission decreased so much that the U.S. declared measles eliminated from the country in 2000.
But this year the U.S. Centers for Disease Control and Prevention has reported 58 measles cases in outbreaks across 17 states—a case number equal to the total measles infections reported in all of 2023. As of last week, the states with documented measles cases in 2024 are Arizona, California, Florida, Georgia, Illinois, Indiana, Louisiana, Maryland, Michigan, Minnesota, Missouri, New Jersey, New York, Ohio, Pennsylvania, Virginia and Washington. The CDC has not reported any deaths, and several outbreaks are still considered active. An outbreak in Chicago that has involved at least 15 cases—several of which were among people staying in a migrant shelter in the neighborhood of Pilsen—has triggered a strong joint response from the city’s department of public health, the CDC and other local health centers to isolate infected individuals and vaccinate people who are susceptible to the disease.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Florida also reported measles infections among several students at an elementary school near Miami last month. The outbreak garnered significant media attention after the state’s surgeon general Joseph Ladapo said in a public statement that unvaccinated children could continue to attend school despite potential for exposure. The Florida Department of Health said that no measles infections have been reported from the school since February 16, although it has not publicized the exact number of cases in the outbreak. The department did not respond to Scientific American’s request for comment.
Some measles transmission each year is expected despite the nation’s herd immunity, which is achieved when the majority of a population—in this case, 95 percent—is immune to a disease. But the high number of infections so early in 2024 has some public health experts concerned about what this bodes for the rest of the year and how vaccine misinformation and disinformation—exacerbated by COVID—may be affecting vaccination rates. “During the pandemic there were obviously a number of people who didn’t like that they were being mandated to receive COVID vaccines, and now that mindset’s spilled over into the [measles] vaccine,” says Offit, who is director of the Vaccine Education Center at the Children’s Hospital of Philadelphia. “But people can forget that measles is exponentially more contagious than COVID..., and it’s a nightmare.”
Measles is an airborne respiratory disease that spreads when a sick person breathes, coughs, sneezes and touches surfaces. Symptoms usually begin 10 to 14 days after an initial exposure. They include a red, splotchy rash that originates on the face and neck, fever, puffy and watery eyes and common-cold-like features. Anyone can catch measles, but children—particularly those two years old or younger with a still-developing immune system—are the most susceptible. There is no specific treatment for measles, and in some cases the disease can cause ear infections, diarrhea, pneumonia and encephalitis (swelling of the brain that can lead to a permanent disability); occasionally it can result in death.
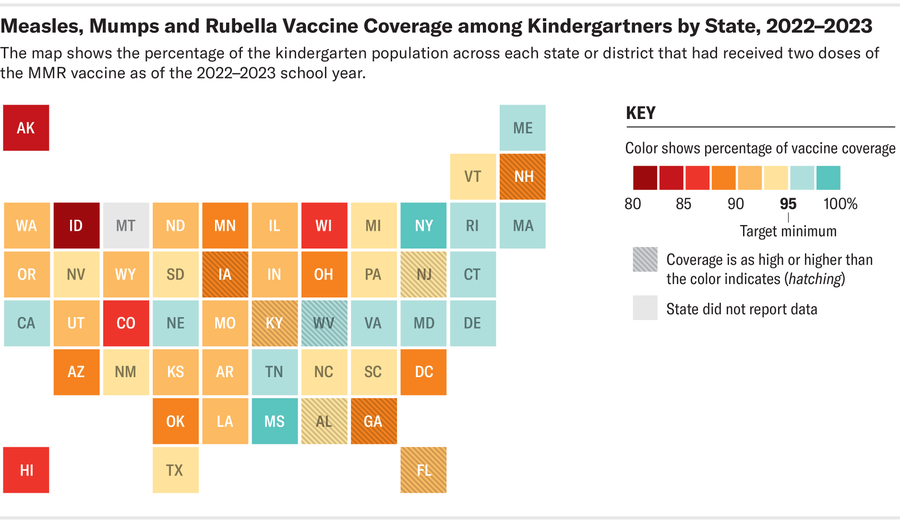
Credit: Amanda Montañez; Source: Centers for Disease Control and Prevention (data)
In the early 1900s the U.S. was reporting an average of 6,000 measles-related deaths each year. By mid-century, developments in medical treatments helped reduce complications and deaths. And people’s natural antibodies, which can be passed from mothers to their babies and provide short-term protection, made infant infections less common. Still, nearly everyone contracted measles by the time they turned 15. Approximately 48,000 people were hospitalized annually, and 400 to 500 died.
“As someone who had a natural measles infection, I can tell you that it’s seriously no fun,” Offit says. “Now they ask old people like me to come down to the emergency room to look at people with fever and a rash because I’ve seen so much of it, and I can tell them within 30 seconds whether or not it’s measles.”
Biochemist John Enders and physician Thomas Peebles created the first measles vaccine, approved in 1963, after successfully extracting and isolating the virus from an infected 13-year-old boy. Microbiologist Maurice Hilleman refined the shot in 1968, and it was distributed across the U.S. This version of the vaccine, called MMR, also protects people against two other infectious diseases, mumps and rubella, and is the shot most commonly used today.
The MMR shot is 93 percent effective at preventing measles, and its use drastically reduced infections. But a notable number of outbreaks were still occurring as of 1989, so at that time, U.S. public health organizations began recommending that people receive one dose of the vaccine around their first birthday and a second dose when they are four to six years old, which provides 97 percent effective protection for a lifetime.
In the early 2000s, however, MMR vaccination rates in the U.S. dipped after British physician Andrew Wakefield published a scientific study claiming that the vaccine could cause autism. His research was debunked after further review but not before it incited fear and skepticism across the U.S. and in other countries. “It’s really hard to unring a bell,” Offit says. “Once people are scared of something, it’s tricky to ease them, and so a bunch of measles started showing up again around 2004 and 2005.”
MMR vaccination rates have been steadily rising since then, and today most public and private schools require children be vaccinated before enrolling. But measles cases are once again popping up around the country, and Offit worries that a surge in antivaccine sentiment that began during the COVID pandemic may be partially responsible.
The most common reasons parents might opt their child out of MMR and other vaccine requirements are for religious or medical accommodations, although some states allow parents to cite personal beliefs as their basis for exemption. According to a CDC report published last November, vaccine exemption rates among kindergartners rose nationally to 3 percent during the 2022–2023 school year—a 0.4 percent jump from the previous year—and in 10 states, more than 5 percent of them had exemptions. Coverage can vary greatly across counties and municipalities, too, says Jerne Shapiro, an instructional assistant professor of epidemiology at University of Florida, and within them, every private institution can also have its own specific criteria for vaccinations.
Measles outbreaks can also start when people who are infected come to the U.S. from abroad. If sick travelers come in contact with unvaccinated or immunocompromised Americans, secondary measles cases can emerge, Shapiro says. One person with measles infects, on average, 12 to 18 others, Offit adds.
With measles outbreaks likely increasing, Offit and Shapiro both urge Americans—especially spring break travelers—to check their MMR vaccination status and seek vaccine and outbreak information only from physicians and government-certified sources, including the CDC, World Health Organization and the National Institutes of Health. “There is so much misinformation about vaccines in general,” Shapiro says. “But this vaccine has been administered for decades and decades. Most of us are fortunate enough not to know what most vaccine-preventable diseases look like, and sometimes we can take that for granted.”
