Balanoposthitis - The International Union against Sexually ...
Balanoposthitis - The International Union against Sexually ...
Balanoposthitis - The International Union against Sexually ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
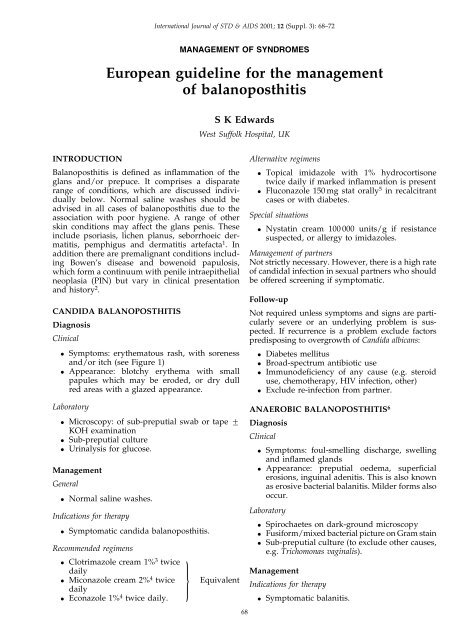
<strong>International</strong> Journal of STD & AIDS 2001; 12 Suppl. 3): 68±72MANAGEMENT OF SYNDROMESEuropean guideline for the managementof balanoposthitisS K EdwardsWest Suffolk Hospital, UKINTRODUCTION<strong>Balanoposthitis</strong> is de®ned as in¯ammation of theglans and/or prepuce. It comprises a disparaterange of conditions, which are discussed individuallybelow. Normal saline washes should beadvised in all cases of balanoposthitis due to theassociation with poor hygiene. A range of otherskin conditions may affect the glans penis. <strong>The</strong>seinclude psoriasis, lichen planus, seborrhoeic dermatitis,pemphigus and dermatitis artefacta 1 . Inaddition there are premalignant conditions includingBowen's disease and bowenoid papulosis,which form a continuum with penile intraepithelialneoplasia PIN) but vary in clinical presentationand history 2 .CANDIDA BALANOPOSTHITISDiagnosisClinical. Symptoms: erythematous rash, with sorenessand/or itch see Figure 1). Appearance: blotchy erythema with smallpapules which may be eroded, or dry dullred areas with a glazed appearance.Laboratory. Microscopy: of sub-preputial swab or tape +KOH examination. Sub-preputial culture. Urinalysis for glucose.ManagementGeneral. Normal saline washes.Indications for therapy. Symptomatic candida balanoposthitis.Recommended regimens. Clotrimazole cream 1% 3 twice}daily. Miconazole cream 2% 4 twicedaily. Econazole 1% 4 twice daily.EquivalentAlternative regimens. Topical imidazole with 1% hydrocortisonetwice daily if marked in¯ammation is present. Fluconazole 150 mg stat orally 5 in recalcitrantcases or with diabetes.Special situations. Nystatin cream 100 000 units/g if resistancesuspected, or allergy to imidazoles.Management of partnersNot strictly necessary. However, there is a high rateof candidal infection in sexual partners who shouldbe offered screening if symptomatic.Follow-upNot required unless symptoms and signs are particularlysevere or an underlying problem is suspected.If recurrence is a problem exclude factorspredisposing to overgrowth of Candida albicans:. Diabetes mellitus. Broad-spectrum antibiotic use. Immunode®ciency of any cause e.g. steroiduse, chemotherapy, HIV infection, other). Exclude re-infection from partner.ANAEROBIC BALANOPOSTHITIS 6DiagnosisClinical. Symptoms: foul-smelling discharge, swellingand in¯amed glands. Appearance: preputial oedema, super®cialerosions, inguinal adenitis. This is also knownas erosive bacterial balanitis. Milder forms alsooccur.Laboratory. Spirochaetes on dark-ground microscopy. Fusiform/mixed bacterial picture on Gram stain. Sub-preputial culture to exclude other causes,e.g. Trichomonas vaginalis).ManagementIndications for therapy. Symptomatic balanitis.68
Edwards. Management of balanoposthitis 69Figure 1. <strong>Balanoposthitis</strong> Ð For all patients: . Advise on hygiene . Look for other STDs . Promote and provide condoms . Suggest partnerattend if symptomatic.)Recommended regimens. Metronidazole 400 mg twice daily for oneweek.Alternative regimens. Co-amoxiclav 375 mg three times daily for oneweek. Clindamycin cream applied twice daily untilresolved.Management of partnersNot strictly necessary. If genital ulcerative diseasepresent, full sexually transmitted infection STI)screening is required.Follow-upOnly required if symptoms do not resolve, or otherSTI suspected.AEROBIC BALANOPOSTHITIS 1DiagnosisClinical. Appearances will vary with the organism,from minimal erythema to ®ssuring andoedema.Laboratory. Sub-preputial culture: Streptococci Group A,Staphylococcus aureus and Gardnerella vaginalishave all been reported as causing balanitis.Other organisms may also be involved.ManagementIndications for therapy. Symptomatic balanoposthitis.Recommended regimens. Depends on the sensitivities of the organismisolated. Erythromycin 500 mg twice daily for one weekwill cover for staphylococcal and streptococcalinfection. Fusidic acid 2% cream 3 times daily will coverfor staphylococci and other Gram-positiveorganisms.Management of partnersNot strictly necessary.Follow upOnly required if symptoms do not resolve, or otherSTI suspected.HUMAN PAPILLOMAVIRUS HPV)BALANOPOSTHITIS 1DiagnosisClinical. Clinical picture of diffuse erythemaLaboratory. Characteristic histopathology on biopsy. HPV detection and typing.ManagementIndications for therapy. Symptomatic balanoposthitis.Recommended regimens. 5-Fluorouracil cream once/twice weekly. Podophyllotoxin 0.15% cream twice daily for 3days per week. Treatment dependent on availability.
70 <strong>International</strong> Journal of STD & AIDS Volume 12 Supplement 3 October 2001Management of partnersNot strictly necessary, although screening for otherSTI would be advisable. <strong>The</strong> patient should beinformed of the riskof transmission of HPV topartners) and barrier protection discussed.Follow-upAssess response to therapy at 1 month. Furtherfollow up only required if symptoms do notresolve, or other STI suspected.LICHEN SCLEROSUSDiagnosisClinical. Typical appearance: white plaques on theglans, often with involvement of the prepuce.<strong>The</strong>re may be haemorrhagic vesicles, andrarely blisters and ulceration. <strong>The</strong> prepucemay become phimotic, and the meatus may bethickened and narrowed.Laboratory. Biopsy: this initially shows a thickened epidermiswhich then becomes atrophic withfollicular hyperkeratosis. This overlies oedemaand loss of the elastin ®bres, with an underlyingperivascular lymphocytic in®ltrate.Biopsy is the de®nitive diagnostic procedure.ManagementIndications for therapy. Symptomatic balanoposthitis. Thickening of the skin on the glans or prepuce.Recommended regimens. Potent topical steroids 7 e.g. clobetasol proprionateor betamethasone valerate) appliedonce daily until remission, then graduallyreduced. Intermittent use e.g. once a week)may be required to maintain remission.Alternative regimensProcedures may be required for speci®c complications,but treatment of the underlying skin diseasewill still be required.. Circumcision if phimosis develops. Meatotomy for meatal stenosis.Management of partnersNot required.Follow upPatients requiring potent topical steroids fordisease control should be followed up regularly.<strong>The</strong> frequency of follow up will depend on thedisease activity and symptoms of the patient, butall patients should be reviewed by a doctor at leastannually in view of the small riskless than 1%) ofmalignant transformation 8 .In addition, patients should be advised to contactthe general practitioner or clinic if the appearancechanges.ZOON'S PLASMA CELL) BALANITISDiagnosisClinical. Typical appearance: well-circumscribedorange-red glazed areas on the glans withmultiple pin-point redder spots, `cayennepepper spots'. This may be similar to erythroplasiaof Queyrat, which is premalignant, andbiopsy is advisable. Patient usually over 30 years.Laboratory. Biopsy: epidermal atrophy, loss of rete ridges,lozenge keratinocytes and spongiosis, togetherwith a predominantly plasma cell in¯itratesubepidermally.ManagementIndications for therapy. Symptomatic balanitis.Recommended regimens. Topical steroid preparations, with or withoutadded antibacterial agents, e.g. Trimovateclobetasone butyrate, oxytetracycline andnystatin) cream, applied once or twice a day 9 .Alternative regimens. Circumcision: this has been reported to lead tothe resolution of lesions 10. CO 2 laser: this has been used to treatindividual lesions 11 Ð no clear evidence onequivalence.Management of partnersNot required.Follow up. Dependent on clinical course and treatmentused, especially if topical steroids are beingused long term. In cases of diagnostic uncertainty penilebiopsy should be performed prior to discontinuingfollow up, to exclude erythroplasia ofQueyrat.
Edwards. Management of balanoposthitis 71ERYTHROPLASIA OF QUEYRATDiagnosisClinical. Typical appearance: red, velvety, well-circumscribedarea on the glans. May have raisedwhite areas, but if indurated suggests franksquamous cell carcinoma.Laboratory. Biopsy: essential Ð squamous carcinoma insitu.ManagementIndications for therapy. Presence of lesion.Recommended regimen. Surgical excision: local excision is usuallyadequate and effective 12 .Alternative regimens. Fluorouracil cream 5% 13. Laser resection} 11 . Cryotherapy 14Management of partnersNot required.EquivalentFollow upObligatory because of the possibility of recurrence.Minimum of annual appointments.Auditable outcome measureOne hundred per cent of patients should have abiopsy.CIRCINATE BALANITISDiagnosisClinical. Typical appearance: greyish-white areas on theglans which coalesce to form `geographical'areas with a white margin. It may beassociated with other features of Reiter'ssyndrome but can occur without.Laboratory. Biopsy: spongiform pustules in the upperepidermis, similar to pustular psoriasis. Screening for STIs especially C. trachomatis.ManagementIndications for therapy. Symptomatic balanitis.Recommended regimen. Hydrocortisone cream 1% or occasionallymore potent topical steroids) for symptomaticbalanitis 9. Treatment of any underlying infection.Management of partnersIf an STI is diagnosed the partners) should betreated as per the appropriate protocol.Follow upRequired if persistent symptoms and/or associatedSTI.FIXED DRUG ERUPTIONSDiagnosisClinical. Typical appearance: variable but lesions areusually well-demarcated and erythematous,but can be bullous with subsequent ulceration. History: a careful drug history is essential, as isa history of previous reactions. Commonprecipitants include tetracyclines, salicylates,phenacetin, phenolphthalein and some hypnotics. Examine the oral and ocular mucosa. Rechallenge: this can con®rm the diagnosis.ManagementIndications for therapy. Symptomatic lesions.Recommended regimen. Topical steroids, e.g. 1% hydrocortisoneapplied twice a day until resolution 15 .Alternative regimen. Systemic steroids may be required if thelesions are severe.Management of partnersNot required.Follow upNot required after resolution. Patients should beadvised to avoid the precipitant.IRRITANT/ALLERGIC BALANITIDESDiagnosisClinical. Typical appearance: very variable. Appearancesrange from mild erythema to widespreadoedema of the penis
72 <strong>International</strong> Journal of STD & AIDS Volume 12 Supplement 3 October 2001. History: symptoms have been associated witha history of atopy or more frequent genitalwashing with soap. In a very small number ofcases a history of a precipitant may beobtained. Patch tests: useful in the small minority inwhom true allergy is suspected.Laboratory. Biopsy: may show non-speci®c in¯ammation.ManagementIndications for therapy. Symptomatic balanoposthitis.Recommended regimen. Avoidance of precipitants, especially soaps 16. Emollients Ð aqueous cream: applied asrequired and used as a soap substitute 15. Hydrocortisone 1% applied once or twice aday until resolution of symptoms.All the above should be used in combination.Management of partnersNot required.Follow upNot required, although recurrent problems arecommon and the patients need to be informed ofthis.References1 Edwards S. Balanitis and balanoposthitis: a review. GenitourinMed 1996;72:155±92 Schellhammer PF, Jordan GH, Robey EL, Spaulding JT.Premalignant lesions and nonsquamous malignancy of thepenis and carcinoma of the scrotum. Urol Clin North Am1992;19:131±423 Waugh MA, Evans EGV, Nayyar KC, Fong R. ClotrimazoleCanesten) in the treatment of candidal balanitis in men. BrJ Vener Dis 1978;54:184±64 Carrilo-Munoz AJ, Tur C, Torres J. In-vitro antifungalactivity of sertaconazole, bifonazole, ketoconazole andmiconazole <strong>against</strong> yeasts of the Candida genus. J AntimicrobialChemother 1996;37:815±195 Kinghorn GR, Woolley PD. Single-dose ¯uconazole in thetreatment of Candida albicans balanoposthitis. Int J STDAIDS 1990;1:366±76 Ewart Cree G, Willis AT, Phillips KD, Brazier JS. Anaerobicbalanoposthitis. BMJ 1982;284:859±607 Poynter JH, Levy J. Balanitis xerotica obliterans: Effectivetreatment with topical and sublesional steroids. Br J Urol1967;39:4208 Bernstein G, Forgaard DM, Miller JE. Carcinoma in situ ofthe glans and distal urethra. J Dermatol Surg Oncol 1986;12:4509 Oates JK. Dermatoses, balanoposthitis, vulvitis, BehcËet'ssyndrome and Peyronie's disease. In: Csonka GW, Oates JK,eds. <strong>Sexually</strong> Transmitted Diseases: ATextbook of GenitourinaryMedicine. London: BaillieÁre Tindall, 199010 Kumar B, Sharma R, Ragagopalan M, Radothra BD. Plasmacell balanitis: Clinical and histological features Ð responseto circumcision. Genitourin Med 1995;71:32±411 Boon TA. Sapphire probe laser surgery for localisedcarcinoma of the penis. Eur J Surg Oncol 1988;14:19312 Mikhail GR. Cancers, precancers and pseudocancers onthe male genitalia: A review of clinical appearances,histopathology, and management. J Dermatol Surg Oncol1980;6:102713 Goette DK, Elgart M, De Villez RL. Erythroplasia ofQueyrat: treatment with topically applied ¯uorouracil.JAMA 1975;232:93414 Sonnex TS, Ralfs IG, Delanza MP, et al. Treatment oferythroplasia of Queyrat with liquid nitrogen cryosurgery.Br J Dermatol 1982;106:581±415 Braun-Falco O, Plewig G, Wolff HH, Winkelman RK, eds.Dermatology. Berlin: Springer-Verlag, 1991:55316 Birley HDL, Walker MM, Luzzi GA, et al. Clinical featuresand management of recurrent balanitis: association withatopy and genital washing. Genitourin Med 1993;69:400±3